Remote patient monitoring (RPM) and mobile remote patient monitoring (mRPM) are forms of telehealth that utilize monitoring technologies tracking patient data beyond the health facility. RPM relies on various technologies to coordinate a multiple-point monitoring system: from source (patient device/sensor), software program (mobile app), the internet, the healthcare provider and finally the cloud/storage system.
Difference Between RPM and mRPM
Often the concept of RPM has become interchangeable with connected medical devices, where data is autonomously transmitted via a network—broadband internet, cellular data, etc.—to its final endpoint. However, there is a difference between mRPM and RPM.
mRPM refers to connected devices that automatically transmit data through the internet or a mobile device via cellular data into a platform that can analyze and view data for therapeutic monitoring. Patients are not required to be confined to one space and there are a reduced number of manual actions needed to collect or transmit data.
RPM can be nonconnected devices requiring patients to report health measures either through a web portal, via telephone, in person with their clinician, or some other manual process. Although RPM is moving more towards a mobilized/connected platform, there still remains a strong population of patients who require access to the nonconnected devices because they are either less expensive and/or patients don’t have access to internet or cellular data.
“RPM is one of those Telehealth modalities that really touches the whole continuum of care. The patient does not have to be in the hospital and now that extends into population health where you can manage the care of multiple segments of patients and effectively manage populations which leads to things like value-based care models. Then there’s the research side of RPM which has so much promise where we’re collecting data, and if we can store and aggregate that data, then we can start doing more predictive analytics and using things technologies such as AI and machine learning to basically make these value-based care systems work.”
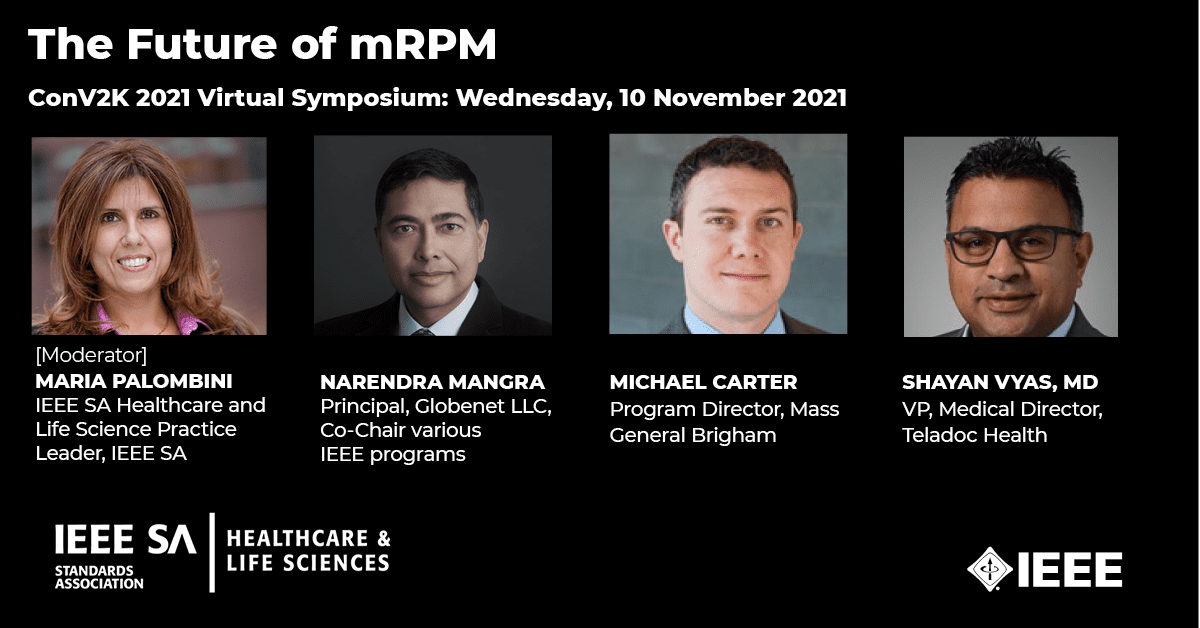
Michael Carter, Program Director, Mass General Brigham;Healthcare Technologies Workstream Leader, IEEE SA Transforming the Telehealth Paradigm Industry Connections Program
The growth in the use of RPM is poised to be exponentially larger in the future with a growing comfort level of use and its ability to treat an expected growing generation of elderly users.
- 30 million US patients, or 11.2% of the population, will use RPM tools by 2024—marking 28.2% growth from 23.4 million patients in 2020
- 703 million people aged 65 years or over in 2019. 1.5 billion projected in 2050. The constant increase in the geriatric population will further support the growth of the remote patient monitoring market
- As of July 2021, Telehealth utilization stabilized at levels 38X higher than before the COVID 19 pandemic.
- 87% of physicians say RPM will be a key part of the patient experience in the future and will most likely double in the next 5 years by 2026.
As the technology developments and use of m/RPM tools continue to grow, new and existing challenges continue to grow alongside it. Many challenges come to mind including:
- With all the innovation in developing and bringing these devices to market, how are we addressing the threats and vulnerabilities to patient’s data security and privacy?
- How are the devices and data interoperable with the rest of telehealth platforms or even the patient’s EHR (electronic health record)?
- How is RPM data delivering more value to the patient in the form of more immediate and appropriate response to potential health issues?
- How are we designing devices and systems that are more inclusive, feasible and adaptable for ALL patients?
“There are a lot of different types of fragmented solutions, maybe proprietary solutions, so we need to get to a point where we are a bit more interoperable. Our devices should be reflective of that; and we understand that there may be different variations and the types of devices and networking capabilities and the types of services that may be offered. But at some point, we want to be able to get to the point where we can communicate seamlessly back and forth, no matter what device or technology happens to be on and no matter what healthcare provider, you are speaking with. That would lead to a seamless overall end-to-end solution.”
Narendra Mangra, Principal, Globenet LLC; Co-Chair of the IEEE Future Networks Initiative (FNI) International Network Generations Roadmap (INGR) and the IEEE Transforming the Telehealth Paradigm; and Co-chair of the IEEE P1950.1 – Standard for Communications Architectural Functional Framework for Smart Cities.
Addressing Opportunities and Challenges Equitably
The IEEE SA Healthcare and Life Science Practice (HLS) is hosting a cutting-edge panel session on Wednesday, 10 November at the ConV2X 2021 Virtual Symposium on the human, technical, and clinical considerations for transforming RPM into a patient-centered care system.
In speaking with this expert and diverse panel, we will get some insight from a technical, application, and clinical point of view on the challenges and opportunities in utilizing mRPM in a way to reach the unreachable with a focus on delivering a human-centered system.
In the course of the discussion, the expert panelists shared the following insights:
- The technical, policy and application barriers when it relates to transferring significant amounts of patient data.
- New applications and potentials for precision medicine that Swarm AI can offer in the drug development process.
- The requirements to drive understanding and wider adoption of the technology in clinical R&D
“When we think about how the healthcare environment was traditionally built on clinicians. There is a waiting room for the physician, why? Because we can’t allow the physician to wait. We want patients to wait for him or her. However, today’s patients, who are everyday consumers, are bringing their expectations from their experience in retail of Amazon or in banking with Bank of America into healthcare…As holistically we think about the one-to-many model eliminating the waiting room allowing patients to access healthcare where and whenever they are ready…”
Shayan Vayas, MD, MBA, Vice President & Medical Director, Clinical Operations, Teladoc Health; Committee Planning Member, IEEE SA Re-Think the Machine Telehealth Competition
Special thanks to our expert panelists who not only dedicate their time to find tools to better enhance patient care but also want to share their insights with the global community to bring forward solutions for trust in adoption of these technologies and applications.
In addition to this special session, the IEEE SA Transforming the Telehealth Paradigm Industry Connections Program is presenting a virtual pitch competition Re-Think the “Machine” Transforming RPM to a Patient-Centered Care System: Solutions Wanted! Learn more about the competition.
If you want to hear the full conversation, join this session to understand what it will take to transition RPM to a patient-centered system that will work for ALL patients.
Subscribe to Win a Free Ticket to Conv2x 2021 Virtual Symposium
We have some full conference complimentary tickets to share with some of our lucky readers. To win this free ticket, subscribe to the IEEE SA Healthcare and Life Sciences Practice Newsletter before 7 November 2021. From 1-7 November, we will have a daily drawing of winners.
Related Resources
- Transforming the Telehealth Paradigm: Sustainable Connectivity, Accessibility, Privacy, and Security for All Industry Connections Program
- IoT Ecosystem Security Industry Connections Program
- Global WAMIII (Wearables and Medical IoT Interoperability & Intelligence) Program
- Ethical Assurance of Data-Driven Technologies for Mental Healthcare Industry Connections Program
- IEEE 11073™ Standards for Personal Health Devices
- IEEE P2933 – Standard for Clinical Internet of Things (IoT) Data and Device Interoperability with TIPPSS – Trust, Identity, Privacy, Protection, Safety, Security
- IEEE 1752.1-2021 – IEEE Standard for Open Mobile Health Data–Representation of Metadata, Sleep, and Physical Activity Measures
- IEEE P1752.2 – Standard for Mobile Health Data: Representation of Cardiovascular, Respiratory, and Metabolic Measures
- WAMIII Virtual Talk Webinar Series
- Global Connected Healthcare Cybersecurity Virtual Workshop Series