Season 4: Telehealth's Quantum Leap into Patient-Centered Care
As a result of the global pandemic, telehealth has become a more comfortable tool for healthcare delivery. The reality is that the way we see telehealth today will look very different tomorrow with more technological innovations and new approaches to administering health beyond the hospital walls. Still, more importantly, it will need to be patient-centered.
Season 4 features conversations with the rising innovators, researchers, policy stewards, clinicians, and industry leaders discussing solutions on accessibility, integration, security, inclusivity, and the other necessary ingredients to migrate the future of healthcare to a patient-centered continuum of care.
Episode 1
Wearing It: Intelligent Physical Rehabilitation
How can we take physical therapy (PT) to the next level using real-world data from tools and devices without having to leave the home?
Josh Rabinowitz, Co-Founder & CEO at Articulate Labs, joins our host, Maria Palombini, in a discussion on a new class of RPM devices that are enabling a viable option for remote patients who do not have access to a facility, but can still rehabilitate with more data and insights to improve their outcomes with or without a certified PT therapist at their side.
Speaker
Josh Rabinowitz
Co-Founder & CEO, Articulate Labs
Josh Rabinowitz currently serves as Co-Founder & CEO for Articulate Labs, a medical device company developing wearable devices to accelerate muscle strengthening and training. In this role, Josh is responsible for fundraising, business development, proposal writing, communications, team/advisor recruitment, and continual corporate improvement. Accomplishments on Articulate Labs’ behalf include multiple awards, letters of interest from hospital systems, risk-sharing partnerships with vendors, pieces of media coverage, and support from nationally recognized health-tech accelerator programs. All the above stem from a drive toward continual improvement in both self and company as a servant leader that starts with unflinching honesty and ends only with quantifiable change.

Full Transcript
Maria Palombini
Hello, everyone! Welcome to the IEEE SA Rethink Health Podcast Series. I’m your host, Maria Palombini and I’m the Director of the IEEE SA Healthcare and Life Sciences Practice. This podcast takes industry stakeholders, technologists, researchers, clinicians, regulators, and others from around the globe to task: how can we rethink the approach to healthcare with the responsible use of new technologies and applications that can afford more security, protection, and sustainable, equitable access to quality care for all individuals. This is an ambitious task, but this is one that we are definitely committed to.
We’re going into our fourth season of the Rethink Health Podcast, and you can look at our other seasons at ieeesa.io/healthpodcast.
So we’re getting into the question of telehealth. As a result of the recent pandemic, the term telehealth has become one of those most frequently used and it does not appear to be going away soon. The reality is that we see telehealth today and it’ll look very different tomorrow. It’s manifesting in many different forms. And it’s not commonly, as we know it, just the doctor and patient experience in some sort of audio/video platform. It has become so much more than that. And I’m sure you’ve heard the term remote patient monitoring or RPMs.
The telehealth experience has changed our expectations as patients on what we can expect on healthcare services. By that I mean, we kind of see it almost like a retail experience, right? We want VIP consierge service, we want amenities, and we want convenience.
And then there’s this growing RPM space. These wearables, these bio sensors in, on, or around the human body monitoring us for some sort of therapeutic condition. There’s so many different forecasts when it comes to the growth of RPM, it could be anywhere from U.S. 150 billion dollars by 2028 and to the idea that a patient might be wearing one or more on their body at any given time.
Here’s what we know, regardless whether we call it telehealth, RPM, mobile health, the future of delivering healthcare is no longer just confined to a facility and it will need to be patient-centered. So, season four. We’re calling it Telehealth Quantum Leap into the Patient-Centered Care.
And this gets to the innovators and the innovators we’re talking to are actually the winners of the IEEE SA Telehealth Virtual Pitch Competition. Plus we’ll talk to industry leaders, clinicians and other researchers who are at the forefront of driving innovation with solutions, looking at accessibility, human factor design, flexibility, interoperability, security, inclusivity, and all the other necessary ingredients to migrate RPM into a patient-centered care system.
So before we begin– a short disclaimer: any of our guests on our podcast series, IEEE does not endorse their products, does not financially support them. We just bring them here for their expertise. And without further ado, I’d like to welcome Josh Rabinowitz Co-founder and CEO, of Articulate Labs. Welcome, Josh!
Josh Rabinowitz
Thank you for having me!
Maria Palombini
Articulate Labs garnered the second place position in the IEEE SA Rethink the RPM Machine Virtual Pitch Competition and their work was on wearable devices for remote direct physical therapy application and monitoring. And we’re gonna get to the core of this in just a second, but Articulate Labs has also placed favorably in other industry competitions, including winning the 12th Annual IOT Wearables Technology Innovation Award, plus a host of others.
So Josh, before we get to the core of the work you do, we’d like to humanize the experience for our audience. So can you tell us a little bit about you? You’re a co-founder of articulate labs, really? What drives your passion in your work and how did you get here?
Josh Rabinowitz
I’ll start by answering the second question first. We got into this quite literally by accident. My co-founder survived a near fatal motorcycle accident some years ago that forced the amputation of his right leg. One of the indirect outcomes of that is that he developed osteoarthritis in the knee of the fully intact leg, the left leg, as he was relearning to walk.
He was advised by his orthopedic surgeon to delay surgery and to exhaust all the conservative options available to him. He found physical therapy to be the most effective means of mitigating the pain and dysfunction that existed in his knee, but he wasn’t able to make it to all his physical therapy sessions.
It was not a lack of desire. It was an issue of time. He had work commitments. He had family commitments, the physical therapy clinic was a half hour drive each way from where he lived. It was a really difficult thing for him to be able to budget time for self care.
He’s a control systems and an embedded design engineer. He’s using a therapy at physical therapy called neuromuscular electrical stimulation. He’s like having these electrical pulses run through the quadrants of muscles around that knee to assist with the restrengthening, the retraining process.
But it’s operating on a pre-programmed sequence and he’s wondering why on earth am I driving a half hour to basically move my leg in time with this thing? Why am I following this technology? Why is this technology not following me? Why is it not adapting to me? It’s kind of what started his development process and figuring out can he make this therapy a little bit more intelligent, a little bit more adaptive.
I got involved as someone who has no engineering or medical background. Just one day randomly looking up knee osteoarthritis and discovering, oh, there’s actually 14 million in the us impacted by this. Not to mention the tens of millions of others around the world with the same condition, not to mention hundreds of millions, around the world, dealing with all kinds of other muscular skeletal conditions.
And we found out, one, this is not a unique situation. We were both operating under the impression this was something that only impacted amputees and two, a lot of other people have the exact same issues of time, distance, reimbursement of existing commitments, all making access to physical therapy very difficult. Realizing those things made us wonder whether the thing that you know was kind of being developed almost as a hobby, as a side project is something that we might wanna really consider sharing with others.
Maria Palombini
It’s interesting that you brought up the unfortunate accident with your partner. As I talk to many more startups, I always find that there is a personal passion behind, especially in the healthcare life sciences sector, why they decided to go with this type of RPM product or that kind of thing. And that’s really where the success is. It’s that passion that fuels that commitment. So this is not atypical from what I’ve heard from other co-founders that I’ve talked to.
So you kind of got into a little bit about what Articulate Labs does. What exactly in your words is the vision of bringing this type of innovative approach to physical rehabilitation, to the healthcare domain?
I’ve been through, like other people, physical rehab for different sort of issues and I agree, going to the facility, getting the appointments, waiting for your therapist sometimes they run late, sometimes they don’t, or you can’t get there. There’s like a whole host of issues that you kind of sometimes feel like it’s almost like a job, right?
Josh Rabinowitz
The mission that’s going to resonate with the greatest population, I think, is going to be convenience. When we think about the act of strengthening the muscle that talking about, well, how do we make this easier? How do we make this more convenient? How do we blend this more into the user’s lifestyle? It is somewhat antithetical so much of the ethos that goes into physical fitness.
That part is difficult, but so much of the issues that we run into with regards to access, is a population of people that cannot budget time for self-care, don’t feel like they can, or don’t necessarily know how to start. And being able to effectively augment movement that they’re going through every day with a proven therapy such that steps walking up and downstairs or getting out of a car, can become strength-building repetitions outside of that physical therapy clinic or gym.
You know, now there’s really an opportunity to help improve access, improve people’s ability to care for themselves on a broader, deeper, longer term. My mission would be in finding ways to talk about the process of strengthening rehabilitation of caring for the body as something that’s for everybody to get outside of the stereotypes or concepts that if you’re not looking like someone who’s showing up at one of the Marvel action movies, then why are you even going to the gym? What’s the point? I think there’s a real need to talk about maintaining your body, because this is your primary vehicle. This is your means to functional independence, to in many cases, to goal achievement, whether it’s travel or caring for loved ones or doing things that you enjoy, you’re having the strength to function the way you want to, not the strength to measure up to someone else’s standards.
Maria Palombini
I think the focus on self care comes in many different forms and I think it is important. Now we’re gonna get to the core of our interview, which is about the innovation. So I imagine your team really got into some heavy research. You probably looked at different models and there’s probably years of work and R and D that went into developing this project.
Maybe could share a little bit of insight with us on what that experience was like and what exactly. But more importantly, I’m really interested to hear what would you consider the most astonishing piece of information that came through in that R and D phase of research for the product?
Josh Rabinowitz
I think the main astonishing outcome and the thing that we’ve had the hardest time explaining to others is that there is no average when it comes to figuring out where people need to be or where they want to be. Especially when you’re talking about people who’ve been coping with and in our case, a knee condition, but really anything on the kinetic chain.
So anywhere between lower back and ankle. When you have an injury in one of these places, you have a tendency to develop compensatory movements as a means to reduce pain in that area. So you might think about the folks we’ve seen in our studies, people who are looking to avoid putting weight on their knee or to avoid extending their knee will develop all kinds of strategies to not use that joint.
Whether they’ll pivot on their other leg, they’ll actually hitch the entire half of their body with the affected knee, they will drag the leg with the affected knee, somewhat behind them. All these things are unique to each individual and the way that these things worsen over time is unique as well.
So every happy gait is the same. Every unhappy gait is unhappy in its own way. Attempting to impose a pre-programmed gait sequence on these individuals and forcing them into a template we found, first of all, it was very difficult to actually trigger the right muscles at the right times.
Going with this average, looking more into relationship between specific quadricep bands and the function of the knee joint during movement, you actually run the risk of exacerbating the condition. If you are strengthening without regard to joint laxity or joint alignment, that really created a need to kind of scrap any sort of template based stimulation, and really start with a form of a model of the joint running on the device that is learning from and effectively distilling movements down into just sets of force vectors as a function of femur and tibia position, motion, acceleration, et cetera. And we really try to just meet the patient where they are. Working with physical therapists to calibrate the device to that user’s gait and to determine which muscles we want to trigger at what times of gait, which movements are problematic, that should be addressed by triggering muscle contraction.
That’s our way to personalize treatment. Something that you said at the beginning that really stuck with me: patient centered care. That’s our opportunity to make truly patient centered care versus imposing our own biases as it were about how a person that we’ve never met should walk.
Maria Palombini
Absolutely. We see this sort of challenge actually transcend the entire healthcare domain. It’s putting patients in a box. I think it’s really important the way you guys got to this level of, I don’t wanna say personalization, but maybe there’s an element of precision on how to use the technology to best support helping these patients.
I imagine our audience might be sitting there and saying, wait a minute, does this mean that we don’t need physical therapists anymore? We know that KneeStim, which is one of your products, is not designed to remove the physical therapist out of the process. But I think the real opportunity is in when you guys describe it is intelligent.
So from your point of view, how can KneeStim really enhance the effectiveness of a physical therapist in working with their patients? I imagine the data capture in the tool can access and utilize. Maybe you could talk a little bit from that point of view.
Josh Rabinowitz
Sure. The first thing we’ve said when we’re talking with physical therapists who might have a little bit of that skepticism first, there’s a lot in the electrical stimulation space and two, there’s been a lot of startups that have marched into clinicians’ offices, kicked in the door saying we’re gonna drag you, kicking and screaming into the 21st century without really paying any attention to their wants and needs. So first I wanna say right up front, we get skepticism and don’t begrudge anyone for it.
The way we manage that is by saying, we’re not looking at this as a means to replace physical therapy. We’re basically taking some of the most mindless parts of your work, which is either setting someone up for electrical stimulation or guiding someone through strength-building repetitions.
And we’re trying to automate that and allow at least some of that work to occur outside of the clinic. Then you can talk about this as a means of improving workflow, saving little bits of time with each patient, as a means to increase throughput ways to maintain a level of communication with the patient that’s not present.
That’s a huge issue. You touched on earlier with regards to your physical rehabilitation experience: 70% of the population that’s prescribed physical therapy don’t show up for all their sessions and are not compliant with their home-based regimens. That represents a financial impact to the physical therapist beyond the altruistic drive to do right by their patients.
When you have a patient that’s not showing up, you’re not earning money. You have a patient that cancels or no-shows, now you’ve got the opportunity cost of having scheduled someone that isn’t gonna pay you and delayed someone that would. With a new remote patient and remote therapeutic monitoring based reimbursement codes, there’s now opportunity for the physical therapist to be able to have some level of visibility on user activity that we’ll be able to measure and report things like steps walked, stride speed, knee range of motion. We’d love to be able to provide a granular level of information to make it clear also what’s happening on stair ascent and descent, or sitting up from a chair, other metrics to make it clear whether someone is making progress in their physical rehabilitation, or if they are at risk of back sliding. By having that data collection and analysis process be reimbursable, now there’s an opportunity for the physical therapist or overseeing clinician to be able to earn some revenue on the patients that they’re not getting to see.
Physical therapists have been really deeply impacted by COVID, in general, just by the increasing difficulty with getting people in the door with decreasing reimbursement for services provided. We see this as a way to be able to provide care and maintain communication while still helping maintain the physical therapist’s bottom line.
Maria Palombini
Yeah, I think for physical therapists there’s a lot of opportunity here with access to data, for sure.
I hear misconceptions around connected wearables and from doctors sometimes they’re like, I don’t know if I wanna use this thing. They’ve got some preconceived notions about them and patients they really know about wearables from the point of commercial fitness trackers, Fitbits, you know, your Apple watches and so forth. What have you seen as the biggest misconception when it comes to these types of applications for connected wearables?
Josh Rabinowitz
Really the biggest misconception I see is really less on the patient or provider side, it’s really in the service provider side. There are a lot of companies in the wearable space and the vast majority of them don’t have to be FDA regulated. They don’t have to really be deeply concerned about security. If they are they’re concerned at a really thin surface level, they don’t have to be concerned about encryption. They only pay a small amount of attention to HIPAA. The misconception I’ve run into that’s been the most difficult to deal with is actually finding vendors to work with on some of this development work that are able to meet the standards for security, for privacy, that are coming, not the ones that are here.
We see Europe as an example of where we think might go over here or at the very least it’s a market that we want to enter in the future and we will need to be able to meet standards for privacy. The number of companies we’ve talked with, who claim to do this work and then have really no idea of anything that’s going on, that’s gonna be necessary for a medical device versus a “wearable” or versus a fitness application. And assuming that we’ve done one, so we can do them all. That’s dangerous. We’ve had to push ourselves to learn what these standards are to really understand them. And then to really grill any potential partner that we meet with on how they intend to meet these standards. And more often than not, we’re kind of met with blank stares.
So I think anyone else who’s in this space, or who’s looking to get into this space I think it’s critical to build up a base level of knowledge of security, privacy encryption, and so forth. I don’t know enough to be able to actually affect anything, but I know enough to be able to challenge and to oversee anyone who’s gonna be doing this work on our behalf.
Maria Palombini
That’s really important. You wanna make sure you have the right partners because overall it’s a brand representation and you have to have it be aligned. Very important point.
You started to scratch the surface of this question a little bit when you first introduced Articulate Labs, but you know, the theme of this podcast is patient-centered. The competition was heavily focused on this idea of transforming RPM into patient-centered system. How do you see your technology being patient-centered from a point, whether it’s from accessibility, visibility, inclusivity, or even just the human factor design? Do you see that there’s a population of patients that you all can better reach and serve with this that maybe they were not accessible before, or they were just resistant to the idea of physical therapy? How do you think you guys are really meeting that idea of patient-centered?
Josh Rabinowitz
I think that element of starting with a very basic concept of how that knee joint is functioning and building the model from the ground up with the user’s own kinematics, with the data coming off of the IMUs, being placed on their legs makes sure that the model that develops is exactly what the patient is what they’re doing. That there’s no concept whether at age, gender, physical ability, that it doesn’t create a conception about what someone does or does not need. It is putting a lot of control in the hands of the overseeing clinician to be able to tailor the stimulation timing and location, and also be able to adjust sensitivity, bias stimulation to one muscle over another, as a means to really make sure that this is hitting the right muscles at the right times at gait, or is contracting the right muscles in time with problematic movements as a way to ideally make those movements a bit easier for the patient.
I think one real interesting possibility that we have here for inclusivity and for access is the ability to provide physical medicine care to people in remote or austere conditions. This is certainly something that is already capable with a lot of the remote or virtual physical therapy options out there and we don’t view ourselves as placing any such service like that. What we see with this device is the ability to really augment and make use of someone’s existing movement. So the people who are in these conditions, they may be like an hour away from a physical therapist. They may be doing work that makes it really difficult for them to set aside even 15 minutes to follow along with a guided physical therapy session. With these populations, there’s an opportunity to use their actions, use their movements and get the same strength-building exercise in without requiring the patient to set aside additional concentration, additional time to change clothing, so and so forth. This is something that ideally will blend in seamlessly into the user’s life and we’re passionate about the possibility of having care, not just augment life, but having it be in support of life. The work that you’re putting in while wearing this device, the strength and reeducation of that muscle that you’re going through is gonna be exactly in line with the things that you’re already doing, the things that you want to do, or the things that you need to do.
I think that’s really intriguing to us and represents a way to integrate physical medicine into people’s lives that hasn’t really been approached previously.
Maria Palombini
I think that’s fascinating. I think this goes a lot into human factor design, the adaptability, the feasibility, these are all really important elements when we’re talking about patients and their physical ailment or condition. I think that’s really an important place and a good place to be in getting your product advocated for. You want patients to say this was the best thing that worked for me. So I think you all are on the right track for sure.
When I talk to a lot of tech startups, they say to me, oh, I wish we had a technical standard for this. Or I wish this was already in place because this would’ve made this part of our work a bit easier. So, do you think there was potentially any technical standards, if any, that would’ve been appropriate or data standard that would made any aspect of developing this product faster, more efficient, easier?
And as you went through the process, did you identify any other areas that you said, wow, this would’ve really opened the doors to innovation in our space, in the RPM space, in the wearable space. And what do you think might be the best way to address it or to go about it?
Josh Rabinowitz
I’ll hit the second question first and say any standard that’s out there, it’s nice to have as a guidepost, but for our purposes, it’s got to be either harmonized or at least asynchrony with the FDA’s doing. If we don’t have the FDA on our side, we’re not selling anything to anyone in this country, at least. And furthermore, the FDA tends to be a gold standard adopted by many other countries that have distributors reach out and be interested in buying our devices.
So getting FDA clearance is not just the gateway to the rest of the U.S. It’s the gateway to get into much of the rest of the world. In that regard, I’d say for us having anything around FDA documentation or standards around use of real time operating systems within a medical device, there’s not a lot of that out there that I’m aware of at the moment.
I could be completely wrong here. But we’re only aware of a small handful of medical specific operating systems, none of which wound up being applicable for what we’re trying to do, because we’re trying to achieve real time application of therapy that does not line up with a lot of existing devices in the medical space that tend to be set up boxes with sets of leads or electrodes or some form of input or output that basically relies on the person remaining stationary. Having more wearable technology means having more firmware that’s operating in a really dangerous space. We’re fortunate standards wise that nothing that we’re doing here really has high risk of ending someone’s life.
But that is not the case if you’re developing a pacemaker or if you’re developing a next generation joint implant. So having frameworks in place for the next realm of operating systems and really having frameworks in place for technologies that are going to be semi-autonomous. And understanding what are the bright lines past, which autonomy cannot be allowed.
There has to be fail safes in place to stop AI from deviating in such a way that it leads to a deleterious outcome for the patient or a potentially fatal one. I think those are the places where right now we don’t see a lot of definition. And we have a path that we see to market based on previously clear devices.
But we also recognize that we’re still looking at bringing something that is gonna be relatively unique to the medical device space. So we’re hoping that us punching through will be an opportunity to broaden the discussion about software and firmware development as we get more into wearables as we get more into decentralized care.
I think inevitably need to start putting more faith or energy or authority in technologies that are gonna be assisting people on medical conditions when a clinician’s not physically present.
Maria Palombini
Absolutely, I think the FDA and EMA depending where you are in the world cannot lose sight. It’s really important to be compliant and under their guise when it comes to anything that you’re gonna use in a medical application.
Josh, you’ve given us so many great insights, especially with the application and what you guys are trying to treat. Are there any final thoughts you would like to share with the audience when you say I’m gonna develop technologies under the context of patient-centered care?
Josh Rabinowitz
We’re actually hosting some students right now in biomedical engineering and one of the most disturbing things that come outta that situation is finding out that they’re looking at adapting, what we’re doing to the knee and fitting it onto someone’s hip.
And they wanted to actually physically prototype the dose, not even adding in electronics, not adding in simulation. Just trying to understand how to get a device to fit around a leg and the professor, as we understand it, basically kinda came screaming into the room to knock the materials outta their hands and said, no, you will only simulate this.
You will never build a single item until run this through whatever simulation package you want. And that makes a lot of sense for like an implant. Trial and error is not a viable there. For something like this, if you’re looking at developing a wearable, then yeah. By all means, try it on yourself.
That’s so much of what we had to do in terms of figuring out a form factor, figuring out how to address corner cases that would exist during gaits such as, you know, stamping your foot or sneezing or stepping off of a curb. Those are only things that we are able to figure out solutions to because we are trying this on ourselves.
For one thing, if you’re not willing to try this on yourself, or if you’re nervous or embarrassed or think about the clinician or the patient that you’re gonna be talking to. How on earth are you gonna convince them if you can’t even convince yourself?
The other thing, going back to the concept of patient-centered care and to some extent, the idea of unconscious bias, we didn’t know what this device needed to do until we had the opportunity to approach the subject with a wide variety of people– different age, gender, size, gait abnormality– all had unique points of view about what they needed out of the device that we would not have figured out and this being founded by two men, a lot of conditions or a lot of situations with women with regards to leg shape– the aesthetics, to some extent, the act of shaving your legs, opening up pores, across which current bridge the gap and create pain.
Those are things we had to learn about from others in the course of controlled experimentation, to make sure that we are developing something that other people would actually want, not just what we would want. So much of this, I think really comes down to experimentation, obviously with full respect and understanding of what the standards are imposed by FDA, understanding institutional review board, how they operate such that when you set up this experiment, you’re doing so in a way that’s ethical and safe.
But you’ve got to be able to try this out and discover problems that you would not have come across otherwise. You’re not gonna simulate your way out of it. You’re not gonna guess your way out of it. The best way is just have someone else break your stuff and tell you what’s wrong.
Maria Palombini
That’s an interesting point. I think here, if I may, maybe the moral of this part of the story is that one size does not fit all. It’s really important because you tend to think, oh, it works here. Let’s just apply. Make a little change and put it here. So really glad you drove that home, Josh.
Josh, I wanna thank you for joining me today and sharing this great insight, the innovation, and the dedication to precision therapeutic that you’re building for this pool of patients. Thank you for being here and sharing that with us.
Josh Rabinowitz
Thank you again for having me. I really appreciate the opportunity.
Maria Palombini
If all of you out there wanna learn more about Articulate Labs, you can visit articulatelabs.tech.
Many of the concepts that Josh and I discussed today are addressed in various activities here at the IEEE SA Healthcare Life Science Practice.
The practice really engages industry stakeholders, such as Josh, around the world to come together and bring these discussions forward. As you notice, Josh already started to allude to that there are some concerns and challenges we have to look at when it comes to autonomous systems and the use of AI. They’re great technologies, but we need some more safeguards there. How can we do this in such a way that we’re gonna really open the doors to innovation and not be a barrier and kind of get this elephant out of the room?
So if you’re interested in getting involved in any of our activities, we have WAMIII (Wearables in Medical IOT, Interoperability Intelligence,) and Transforming the Telehealth Paradigm, which are Industry Connections Programs and they’re really getting to the core of all these connected technologies being used in a remote environment to address patient’s needs with privacy security, the flexibility, the human factor design– they’re attacking all these issues. If you wanna find out more about the work of the practice and all these individual programs I mentioned, please visit us at ieeesa.io/hls.
If you enjoyed this podcast, if you enjoyed the conversation or found something useful in this tidbit of insights that were shared with you today, we ask you to share it with your peers, your colleagues, or on your networks.
This is the only way that we can get these important information out into the domain to talk about the important work our volunteers are doing in the Healthcare Life Science Practice. So please use hashtag IEEE HLS or tag us on Twitter at IEEE SA or on LinkedIn, the IEEE Standards Association when sharing this podcast.
I wanna thank all of you for joining us today and listening in, continue to stay well and until next time!
Episode 2
Breathing New Opportunity: Keeping Asthma Patients Connected
Breathing is essential; how we breathe is just as important. RPM tools offer an amplified opportunity for visibility for those with chronic conditions such as asthma. A majority of asthma sufferers are children, which means monitoring and getting real-time understanding of their condition is that much harder.
JC Ren, Assistant President at CMI Health, shares how the latest RPM tools offer both real-time monitoring to parents and caregivers while making it convenient for children to utilize to help better monitor their condition.
Speaker
JC Ren
Chief Operations Officer, CMI Health
JC Ren is the Assistant President of CMI Health. He is involved in many key aspects of the company, including new product development, sales, 2B tech support, regulations, and daily operation. JC is also project lead of CMI Health’s new AsthmaGo solution.
JC has been with CMI Health since 2015. Prior to joining the company, he earned a Master’s degree in electrical engineering from Georgia Institute of Technology, and a Bachelor of Engineering degree in Electrical Engineering from Vanderbilt University.

Full Transcript
Maria Palombini
Hello everyone and welcome to the IEEE SA Re-think Health Podcast Series. I’m your host, Maria Palombini. I am the director and I lead the Healthcare and Life Sciences global practice here at the IEEE SA. This podcast series takes industry stakeholders, technologists, researchers, clinicians, regulators, and more from around the globe to task and we asked them: how can we rethink the approach to health with the responsible use of new technologies and applications that can afford more security, protection, and sustainable, equitable access to quality care for all individuals, you can check out our previous seasons on ieeesa.io/healthpodcast.
As a result of the recent pandemic, the term telehealth has become one of the most frequently used terms and it does not appear to be going away. The reality is the way we see telehealth today will look very different tomorrow. Telehealth is manifesting in many different forms. It’s more than what we commonly see as the doctor/patient exchange on an audio or video platform and it continues to grow with the use of RPM, remote patient monitoring devices. The telehealth experience has changed the patient’s expectation on healthcare services. They’re relating it to more of a concierge-level retail experience: convenient, appropriate, and in-person.
There is a growing RPM space. There are many forecasts about RPM devices- anywhere from US 150 billion by 2028 to estimates that 40% of patients will be utilizing one or two of these devices at one given time. But there’s one thing for certain, regardless if we’re talking telehealth, mobilized health or RPMs, the future of delivering healthcare is not confined to a facility and it will need to be patient-centerED.
Season four of this podcast series, Telehealth’s Quantum Leap into Patient-centered Care, talks to the innovators. These are the winners of the IEEE SA Telehealth Virtual Pitch Competition, the industry leaders, clinicians, and other researchers who are at the forefront of driving innovation with solutions on accessibility, human factor design, flexibility, interoperability, security, and a whole host of other necessary ingredients to migrate healthcare in the form of telehealth to a patient-centered care system.
So a little short disclaimer, before we begin: IEEE does not endorse or financially support any of the products or services discussed by our experts in this series. And with that out of the way is my pleasure to welcome JC Ren, Assistant President of CMI Health, Inc. Hi, JC!
JC Ren
Hi, Maria. Thank you for having me. It’s an honor to be here.
Maria Palombini
Absolutely. So JC and CMI Health are the producers of a device called AsthmaGo. It’s an RPM device. AsthmaGo is a HIPAA-compliant asthma solution that consists of smart home use medical devices, a mobile app, and a physician dashboard. AsthmaGo is a great innovation.It placed third in the IEEE SA Re-think the RPM Virtual Pitch Competition.
So we’re gonna get to the details of the innovation because innovation comes with a solution. But before that, JC, can you tell us a little bit about you? You’re Assistant President at CMI Health. What drives your passion to work at this organization?
JC Ren
So CMI Health is a startup company. We specialize in medical devices, both clinical and for consumers, and we are a relatively small team but we really make a big impact in the industry. And then to all of our customers, it’s really a great industry to be in healthcare as well as we are highly involved in the telehealth and the RPM sector. So it really feels good to know that our products are helping people and improve their life quality, improve their medical outcomes.
It’s a good feeling to read all those customer reviews online, like the Amazon store to learn about how our products improved their life.
Maria Palombini
Absolutely. You know, I’ve interviewed quite a few innovators, especially the entrepreneurs and there seems to always be a human story behind their innovation, their products. When it comes to AsthmaGo, can you share with our audience, what was the driver behind the development of it? Was this shaped by perhaps a co-founders own experience with a friend or family member or maybe something they were exposed to while they were doing undergraduate work at a university? What was the driving motivation of bringing this product to the market?
JC Ren
I first started to learn more about asthma when I was in grad school. I did a small project when I was at Georgia Tech. It was a children’s hospital project with child asthma. That’s how I started to recognize this huge population, how severe it is. But the actual story behind this is one of our partners had a conversation with his golf buddy and his friend has a son with asthma. He’s really worried about his son’s sleep because sometimes there might be an attack or sleep disorder caused by the asthma condition. So he’s really worried that he cannot fall asleep. He has to get up and see his son so he really wanted something to monitor closely every night. During the sleep you wanna know his son is okay so both him and his wife feel safe.
Maria Palombini
Unfortunately, we hear more and more about children suffering from asthma for many different reasons. And of course, I imagine that brings a lot of stress to parents everywhere in the world.
So to our audience, now we’re gonna get to the core of our interview, the innovation. Just food for thought: RPM, remote patient monitoring, is more than just a device and a telemetric way of transporting information. It has to be a care system that is built around not only the patient’s therapeutic condition, but also their social and other home determinants. And JC just started to allude to an exact use case when it comes to children in the home and fear of quality of life and worrying. Your child is not breathing right. And all these kinds of other issues. We know that according to the World Health Organization, asthma affects an estimated 262 million people.
And that was in 2019 and caused 461,000 deaths. So this is not something that we can just push to the side, right? It is a non-communicable disease that affects both children and adults equally. So JC, how does AsthmaGo support this very large and diverse population of patients?
JC Ren
Asthma is like a typical chronic disease, so being like a chronic patient. So it’s more like a lifestyle. Everything in your life is being influenced by the conditions and there’s such a huge population. So we keep in mind that the key concept is we want to help the patient to manage asthma at home. That’s where they spend most of the time- at home.
But at the same time, they have to fight this condition. If it’s managed properly, it can minimize the impact. So we are empowering the patient and putting them in the driver’s seat of asthma management. So to accomplish that, we use this simple and very user-friendly mobile app. Because, everyone has a smartphone and that’s becoming part of everyone’s lifestyle.
So we just use the mobile app. So making it like the morning routine or something that is at their disposable anytime, anywhere. And then we also have those over the counter devices that’s really affordable and easy to use and to care that way they can do the test anywhere. And then know their vital readings so they can know early, if anything goes wrong, if they need to use a medication, they need to see the doctor by doing all that very conveniently and right out of your pocket solutions.
We can prevent a lot of the exacerbation and ER visits from happening, greatly improve their quality of life, and reduce the cost.
Maria Palombini
Absolutely. I think that you’re right. It’s a really good way of saying that asthma is a chronic condition and it’s just not gonna go away with a simple antibiotic. It’s living with a lifetime condition.
So you mentioned this a little bit before in your intro, when you were doing your studies, you were exposed to people with asthma, children. Can you share with our audience a little bit about the types of research, the modeling, and the years of work and time that went into developing this product? And in that research, what would you say was the most interesting thing that came out through this research and development phase of this product?
JC Ren
So let me start from our company, how we get started. One of the founders, he has 30 years of experience in the medical device industry, particularly in the respiratory area, like CPA machines, things like that.
We started in the oximetry business, like oxygen monitoring before we developed this product. We do a lot of sleep apnea monitoring because the patient’s oxygen will fall rapidly during sleep because their breathing stops. So the solution can develop from there. We have some manufacturing partners that are specialized in spirometry devices and they try to make something that’s very affordable and easy to use at home because we found it’s really difficult for the patient to manage this condition at home. Most people rely on doctor’s visits maybe once a month or so and that’s clearly not enough. So we have developed this spiraling device, that over counter spirometry, and we developed it, using a different technology that’s a pressure sensor different from the traditional turbine, which is derived from a hospital grade desktop unit. And at the same time, it’s easy to use and to maintain lower cost than the common units in the market.
So that’s how we developed one of the key devices to bridge the gap and appeal to a huge population without compromise, like accuracy or reliability. That’s how it starts and we also combine our specialty, right? Oximetry, so the patient or the child can be monitored continuously throughout the night, lowering the risk or the parents worry that something may happen during the night.
Maria Palombini
Absolutely. This is a nice segue to my next question. So we know that asthma is a common chronic disease among children, unfortunately. And like you said, parents are worried, right? They’re worried about when they’re sleeping and they’re getting enough oxygen. Obviously there’s a lot of concern there, but we also know that children are traditionally not the best at patient adherence- they’re children. They’re like, I don’t wanna wear this thing. I don’t wanna touch this thing. Their mind is in a million other places. So how do you find children using this product? Do you find that they’re compliant, that they’re using it correctly? They’re using it at the specified times they need to use it? Do you find that parents are not complaining? Oh, my child doesn’t like to use this thing. WHat are you finding in that specific area of opportunity and working with children?
JC Ren
Yeah. So we actually have this in mind during the whole kind of development process. So for example, our spiral link spirometry device has a really nice and narrow mouthpiece opening.
So that’s gonna be easier for the children to blow into it. And also for the oxygen monitor. Our oxide watch, we have a kids version. So for adults, they have a big finger sensor, but we have those little fingers with nice colors, like a bright blue color or pink color for the kids and with a tiny little finger sensor.
So our product has age groups and also for the children. We’re also working with some groups, trying to set up studies for children, to see their compliance and to see the best way to improve adherence. And then the outcome. There are many ways to get there, like things that appeal to children, like better UI design of the app, or even like the daily routine testing, more fun things like those. We don’t have the final product yet, but we are in the kind of active process of developing.
Maria Palombini
There are so many devices we talked about, they’re coming into the market in many therapeutic areas, many different applications and so on, but we’re seeing sometimes this one hit, I call it a one hit wonder approach, right?
We’ve developed this device. We put it on the market. It’s a monitoring device. It can connect to an app. It can collect and transmit data. And then we have to wait. The next version comes out for it to do the next thing. And you start to talk about, this is the interesting point of your particular innovation.
It’s scalable and extensible. And I wanna get your point of view when you were developing this RPM device, why did you find it important to have that in the product design and how did you feel that would best serve the patients that you’re trying to help?
JC Ren
Yeah, I think the key concept and the thing we always think about is the patient. So our goal is driving the patient, motivating the patient, making everything accessible and then convenient. So they have everything they need and they can do it very easily. And then, we don’t focus on one specific device. We think about it as a whole concept, the whole idea, a solution to help people with asthma.
So one thing we keep adding different devices. So it’s like different tools for the patients at home, at their disposal. For example, like a brace trainer because managing the disease testing is one thing the recovering/training exercise is another important part of this condition like chronic disease and also like inhaler, counter.
So many of these will play a critical part in the patient’s life. So we can try to make their life easier, not only just focusing on one device. We’re focusing on the patient and also with the API and SD case of our devices, all these great devices that we have are not only available to us. It’s literally available to everybody. So say like another company, like RPM or telehealth group, they have a specific need. Whether it be for seniors, for children and they have some other great solutions and our device is available to a company like this so they can make these great user friendly devices as part of their solution.
We are also helping the patients like the end user and also the industry, so many other companies. There’s a lot of different solutions and products available for different scenarios.
Maria Palombini
When you think of the patients that can benefit from the technology CMI has developed, how do you see it being patient centered from a point of view of accessibility, adaptability, flexibility, or those areas of interest? What are some of the outcomes you have seen with the ability of doctors to have access to the real time data coming from these devices to enhance the patients’ care?
JC Ren
If you think about the patient care, especially for this chronic disease, actually the patient can spend 90% of their time with themselves at home or with family, not with a doctor. So they are responsible for the most part, for their own care. The patients are actually the best caregiver for themselves. If they’re equipped with the correct tools, mindset, and the knowledge. We want to bridge this gap of traditional patient care. Traditionally it’s like taking photos. Patients go to doctors once at a time, but the doctor only sees photos of the patient. They don’t know what happens at home. Maybe there’s an asthma attack. There’s some trigger or some feeling the patient doesn’t even know themselves. They cannot describe it or they forget when they’re at the doctors. With telehealth and RPM solutions, like our AsthmaGo, it’s more like taking a movie that’s continuous. It records everything that happens all the time. And the doctor now has access to this movie. So the trend is very clear. They will know a lot better about the patient. Maybe the medication is not bad or maybe some other factors like weather or activity influence the condition. So it’s a lot easier for the doctor and the patient to improve the outcome, because the patient is responsible for their own care. So we try to give them the best they can have at home so they can take charge. That’s what we say, that we put them in the driver’s seat. And by doing that, we are actually promoting early prediction and early intervention. So we believe that’s the best way for all this type of chronic disease, because there’s no severe tax ER visits that will result in better quality of life and better outcome and lower cost.
Maria Palombini
Absolutely. I agree. I mean, I think that there’s so much here, you know, the opportunity for patients to definitely take control of their condition, you know, using great tools, such as these and others out there.
I talk to many different tech entrepreneurs, a very exciting opportunity to hear from them. And they always mention to me, in the development phase or in the research phase, they’re like, wow. Had this technical standard or data standard been in place, it would’ve been a huge help or policy sometimes be written in such a way it would’ve made things a lot easier.
So my question to you is after going through this development process and going through this whole experience, what are some of the things that you guys experienced? If we had this, it would’ve made it easier. And how do you see that potentially opening the doors to innovation in this RPM space? If that challenge still exists, how do you guys think maybe there’s a better way to address it?
JC Ren
This is a big topic. Maybe I’ll just talk about one part of it. That’s the connectivity. That’s the fundamental basis of telehealth. We want the doctors or the nurse caregiver to be able to access patient data, be able to communicate and provide care remotely.
So connectivity is key. The IOT device that’s equipped with Bluetooth technology, wifi cellular. That’s really important. And throughout our development process or the years in business, we also find out the cellular starts to play a more important role and then become convenient compared with Bluetooth and wifi. Because sometimes you’re dealing with little kids or seniors. Sometimes we have to skip the mobile connection due to personal reasons. But cellular connectivity can really close somefinal mileage. For example for seniors, for like remote areas, things like that, with no wifi.
And we are actually moving toward a lot of cellular enabled devices and then trying to keep all of our patient customers connected wherever they are.
Maria Palombini
I think that’s a really good point. I think keeping patients connected and we hear connected healthcare everywhere, keeping them really connected means more than just connecting them to their device and that’s it. It’s the whole experience across the continuum of care.
So JC, I think you’ve given us some really interesting thoughts. I mean, obviously you guys are tackling a significant global chronic condition through the use of this. Are there any final thoughts you would like to share with our audience as technologists who’re looking to develop a device in the RPM space to even go into some support of chronic conditions or just this idea of design mindset, patient-centered care. What advice or thoughts would you share with our audience on that?
JC Ren
Maybe just some quick points for both patients and for doctors, you’ll find a lot of great innovations and great convenience.
If we can try new things, try new technologies. I know it’s typical in the healthcare industry, because we have many hospitals and doctors. They prefer more traditional ways of doing things. We’re gradually moving toward the technology trend, but we are still years behind what actually the technology develops, but we are heading toward the right direction, especially as we are in the COVID situation in the future post COVID.
And we have a lot of these great regulations, reimbursement, everybody starts using and accepting the idea of telemedicine, telehealth using their mobile and doing things they are not able to do before at home. And suddenly we’ll find out, oh, that really makes our life easier.So, yeah that’s what I want to add.
Maria Palombini
Absolutely. So for all of you out there, trying to get into the telemedicine space, you have to think about patients from multiple different ways, just not their clinical therapeutic condition. And that’s a really important point. So JC thank you for joining me today. It’s been an absolute pleasure, hearing more about AsthmaGo.
JC Ren
Thank you, Maria, for having me.
Maria Palombini
If you wanna learn a little bit more about AsthmaGo and overall CMI Health, you can visit cmihealth-inc.com. If you like to see the finalist pitch videos from the Rethink the Machine Virtual Pitch Competition, they’re available on the event website at ieeesa.io/telehealthcomp.
Many of the concepts in our conversation with JC today are addressed in various activities throughout the healthcare and life science practice here at the IEEE SA. The mission of the practice is engaging multidisciplinary stakeholders and having them openly collaborate, build consensus, and develop solutions in an open standardized means to support innovation that will enable privacy, security and equitable, sustainable access to quality care for all.
There’s so many different activities here, such as WAMIII, the wearables of medical IOT, interoperability and intelligence global incubator program, the transforming the telehealth paradigm industry connections program and all of these different areas of accessibility, human factor design, seamless connectivity are all being addressed by our volunteers.
So if you’re interested and you wanna learn more about these projects or all the other additional projects, which I didn’t even get a chance to mention, you can visit the practice website at ieeesa.io/hls.
If you enjoyed this podcast, we ask you to share it with your peers, your colleagues on your networks. This is the only way we can get these important discussions out into the domain is by you helping us to get the word out. You can use #IEEEHLS or tag us on Twitter at @ieeesa or on LinkedIn at IEEE Standards Association when sharing this podcast.
Special thank you to the audience for listening and being here with us today. Continue to stay safe and well until next time.
Episode 3
Getting a Hold of Chronic Conditions for Patients in Developing Regions
Patients in developing regions are most often the most underserved populations whereby chronic conditions are left unchecked as a result of inaccessibility to health care, facilities, or tools. IEEE Student Member, Pramuka Sooriyapatbandige, shares how his research team is looking to mitigate the issue of accessibility with a simple, yet multi-purpose RPM tool that can be utilized, accessible, and feasible for patients in developing regions.
Speaker
Pramuka Sooriyapatbandige
IEEE Student Member
Pramuka Sooriyapatabandige is a final year undergraduate student at the University of Jaffna, Sri Lanka specializing in electrical and electronic engineering. He is a student member of IEEE and the Institution of Engineers, Sri Lanka (IESL).
Pramuka is a member of the research team working on the project “Multi-Purpose Health Monitoring Bracelet,” a low-cost wrist wearable bracelet that makes remote health monitoring easily accessible for anyone. The project was placed first in the student/academia category of the IEEE SA Telehealth Virtual Pitch Competition 2022 – ReThink the Machine: Transforming RPM in a Patient-Centered Care System.

Full Transcript
Maria Palombini
Hello everyone. I am Maria Palombini and I am the Director of the Healthcare and Life Sciences Practice here at the IEEE Standards Association and welcome to the Re-think Health Podcast Series. This podcast takes industry stakeholders, technologists, researchers, clinicians, regulators, and more from around the globe to task: how can we rethink the approach to healthcare with the responsible use of new technologies and applications that can afford more security protection and sustainable equitable access to quality care for all individuals? You can check out our previous seasons on ieeesa.io/healthpodcast.
So as a result of the recent pandemic, the term telehealth has become one of the most frequently used ones and it doesn’t appear to go away soon. The reality is that we see telehealth today will look very different tomorrow. It’s manifesting in many different forms. It’s more than what we see in the doctor/patient exchange on an audio video platform. It continues to grow with the proliferation of RPM devices, remote patient monitoring devices.
And we see that the telehealth experience is really being changed by the patient’s expectation on healthcare services. They are more relating it to a concierge level of online retail experience, convenient, appropriate, and personalized. With the growing RPM space, there are so many different forecasts when it comes to this, it could be U.S. 150 billion by 2028, or that more than 40% of patients will be utilizing one or two of these devices at one given time.
But here’s one thing we know for certain, regardless if we’re seeing telehealth, mobilized health, or RPMs, the future of delivering healthcare is not going to be confined to a facility and it will need to be patient-centered. So season four of this podcast series, Telehealth’s Quantum Leap into Patient-centered Care talks to the innovators.
These are the winners of the IEEE SA Telehealth Virtual Pitch Competition. We talk to the industry leaders on the platforms leading the way, clinicians, and other researchers who are at the forefront are driving innovation with solutions on accessibility, human factor design, flexibility, security, inclusivity, and more.
These are all the necessary ingredients to migrate telehealth care to a patient-centered care system. Before we begin just a short disclaimer, IEEE does not endorse or financially support any of the products or services discussed by our guest experts in this series. With that out of the way, it is my pleasure to welcome Pramuka Sooriyapatbandige, a final year undergraduate student at the university of Jaffna in Sri Lanka, specializing in electrical and electronic engineering.
He’s a student member of IEEE and he also placed first in the student category with his project, Multi-purpose Health Monitoring Bracelet in the IEEE SA Virtual Pitch Competition: Rethink the Machine – Transforming RPM in a Patient-Centered Care System. Pramuka, welcome to our podcast.
Pramuka Sooriyapatbandige
Thank you
Maria Palombini
Pramuka, before we get to the core of the innovation, we like to share with our guests a little bit about the person behind the technology. So can you tell us a little bit about your research work and how you and your team came together to develop this project?
Pramuka Sooriyapatbandige
Yeah. With the COVID 19 pandemic, Sri Lanka University started to explore possible supports that could be contributed to manage the pandemic situation in the country. And during this period, we also needed to identify the research project to fulfill the requirements of our undergraduate course.
And this is when Mr. Valluvan, who is our current supervisor, proposed the idea of RPM, and we started working together. It seemed very time appropriate and aligned with our research interests. Also, we were able to get the assistance of Dr. R. Surenthirakumaran and Dr. Sivasothy, who were already contributing to some of the university’s initiatives during the pandemic time. They helped us develop the concept further.
Maria Palombini
Excellent. I find that most of the time, when I talk to technologists/entrepreneurs, there’s always a motivation, like a life story or some sort of passion that drives them to develop this innovation, this technology. Can you share with us maybe something you and your professor, your team members, something that was the real motivation to really take this project to the level and try to make it accessible to the underserved populations in developing regions?
Pramuka Sooriyapatbandige
The motivation for this project comes from what we saw and experienced around. Globally, non-communicable diseases, cardiovascular diseases, cancer, diabetes, and chronic respiratory diseases account for over 70% of deaths. And three quarters of all NCD deaths occur in lower and middle income countries. And nearly 85% of global premature deaths from NCDs are reported in these countries, whether developing countries, Sri Lanka faces similar issues as other low middle income countries, where some problems are unique to Sri Lanka. NCDs are estimated to account for 75% of total debts in Sri Lanka with nearly one in five people dying prematurely from NCD.
These NCDs tend to be of long duration and have characteristics of insidious onset, chronic clinical manifestation, and long-term disability in the face of poor control. And most patients with NCDs are diagnosed in later stages, particularly after developing serious symptoms or complications. So in October, 2015, the United Nations Interagency Task Force on NCDs conducted a mission to Sri Lanka and it concluded that epidemic of NCDs has become a serious economic and public health issue in the country. And it’s fueled by tobacco use, unhealthy diet, alcohol consumption, and physical inactivity. The health system of Sri Lanka is considered a highly successful low-cost model. It is widely accessible and it has services offered by the public healthcare system, are free at the point of delivery, and other factors like wide coverage, female literacy have resulted in remarkable health indicators in the country. However, strengthening primary healthcare with comprehensive community based and family focused care, it’s the solitary solution to address the existing health issues in Sri Lanka.
So we believe that home-based monitoring of the essential health parameters is very important and that growing technology should address this need. So we thought our solution would be suited for this purpose. So this is actually the motivation behind our project.
Maria Palombini
Very fascinating and very important. So now we’re gonna get into the core of the innovation. We know for patients with chronic NCDs, non-communicable disease conditions, without easy access to healthcare, RPM, remote patient monitoring devices may be the lifeline they need to minimize risk of urgent hospital visits or other unplanned clinical visits and especially when we’re in developing regions, it’s not like there’s hospitals and clinics easily accessible to your “fingertips,” as we say. For individuals in developing regions RPM devices that are accessible (and accessibility can come in many different ways) can be a significant contributor to improving their health.
So Pramuka, what stage is the multipurpose health monitoring bracelet? Is it a concept or is there a prototype, have you had any testing in the form of a pilot done with it? What are some of the findings? What’s actually going on with this particular product right now?
Pramuka Sooriyapatbandige
Currently, we have the proof of concept prototype and we are in the process of making the final prototype, which is pilot-ready.
Maria Palombini
Can you share with us the type of research you all did, the modeling, maybe levels of work that went into actually refining this proof of concept prototype? And what would you say was the most interesting piece of information that came through in this research and discovery phase of the product?
Pramuka Sooriyapatbandige
Certainly. At first we looked into the requirements and it was quite a challenge as we had minimum exposure to the biomedical field. When identifying requirements, we had to study the vital signs, how they’re measured and existing technologies. We also looked into existing RPM solutions. As we were looking into developing a wrist wearable device, we realized that all our measurement requirements could not be fulfilled by the wrist wearable device alone.
And this is where we came up with the capability to connect add-on devices. Initially, we intended to measure a set of limited measurements and vital signs. But we were astonished that the capability to connect add-on devices would give our device the unlimited expansion of measurements, making our device the hub or centerpiece of a remote health monitoring system.
For the development, we followed the modular approach where we developed and tested different functionalities separately and later put them together as one device.
Maria Palombini
That’s fascinating. So you all are developing a device that’s accessible, right for a developing region, but also now it’s scalable.
So, can you explain how it can interoperate with other devices, such as a pulse oximeter, a blood pressure cuff? Does it require that a specific type of device can connect with the bracelet or is it the multi health monitoring bracelet that can work with any device by any manufacturer?
Pramuka Sooriyapatbandige
When building the multipurpose health monitoring bracelet, we studied the capability and size of the sensors that can be used for medical purposes. And if the sensor cannot be accommodated within the bracelet or measurement cannot be made at the wrist, we tried to use wireless connectivity, such as Bluetooth to connect the measurement device and bracelet. Therefore the bracelet gets the capability to include additional medical measurements. So when using BLE wireless connection, BLE generic attribute profile (GATT) is a better choice.
It is standard-based and this profile helps interchange data between two BLE devices. Manufacturers can implement those profiles to communicate with MHMB, for example, already some profiles, blood pressure, heart rate, pulse oximeter, insulin delivery service, low-cost profiles are available in BLE standard organization and existing devices can be easily modified to include this capability.
Maria Palombini
Great. Obviously we see so many new devices coming into the market, but unfortunately they don’t really integrate with many other things or they’re not scalable or extensible. So this is really important. I think this can be a significant attribute, especially to a population who doesn’t have so much access to healthcare.
Pramuka, one of the biggest challenges we see in remote patient monitoring, is the issue of accessibility. And like I said earlier, accessibility can mean a whole bunch of things could be from a point of view that people can’t afford. It could be that people don’t know how to use it, because it’s too technical. It could be a whole bunch of things. So I know that you mentioned that one of the main features of the MHMB is that it is accessible, especially to individuals in developing regions where they don’t have easy access to healthcare. So in helping that population of patients, what makes it so accessible?
Is it that it doesn’t require high frequency bandwidth, like consumption of data or internet, or is it something that can easily communicate? It’s very easy to use. What makes it accessible for this population?
Pramuka Sooriyapatbandige
Our device stores data locally when not connected to the internet and pushes to the cloud, as soon as it is connected again. So during this period, local analytics, which run on the device can help alert the use of abnormal measurements. So it performs basic functionalities, even in the absence of a network connection. And the device is simple. It does not require any special training. Also it does not have a display and requires minimum attention from the wearer, therefore minimizing its impact on the daily lifestyle of the wearer. I should also mention that we identify our device as a low-cost device.
Maria Palombini
Fascinating. We know that there’s a whole market of consumer driven fitness wellness devices that they say they can track your heart rate, your blood pressure, your activity level, your oxygen level. It can do all these things. What makes the MHMB different? Why a physician and/or a patient should trust that this device can be utilized to help their clinical health outcome.
Pramuka Sooriyapatbandige
This is a good question. First of all, we recognize MHMB as a clinical device, rather than a fitness or wellness device. It is a part of an entire remote health monitoring system, unlike most fitness and wellness devices. It is developed focusing on clinical requirements as its primary function. And we intend to release and get the approval of relevant authorities to identify it as a medical device.
And most importantly, MHMB has unlimited measurement capabilities due to their ability to connect add-on devices via the MHMB to a single health monitoring platform, which is not afforded by any other device.
Maria Palombini
I think this is a very important distinction, especially for patients and physicians to know this as well.
Were there any technical or data standards, if applicable, that would have made aspects of developing this concept faster or easier? After going through this process, were there areas where you would say, had we had this, it could really open the doors to innovation and especially in this RPM telehealth space? In your opinion, if there’s still these challenges, what may be one of the best ways to address it?
Pramuka Sooriyapatbandige
Yeah. The standard communication protocol among devices generating medical data would have helped make the process of development more convenient and efficient. Also a common development platform specifically designed for medical and health monitoring purposes would further open doors to the innovation in telehealth space.
An open source development platform would be able to get community contributions to accelerate the process of developing remote health monitoring devices.
Maria Palombini
I’ve heard before that the open source platform is a really important aspect for tech developers.
Pramuka, you’ve given us some really interesting insights. This is a fascinating concept prototype. We definitely are interested to see and to know when you’re going to do your pilots and how the outcome comes. But in the meantime, are there any final thoughts you would like to share with our audience? When it comes to developing technologies, specifically, if you’re going to target underserved patients in developing regions?
Pramuka Sooriyapatbandige
The key is to have the right partners and parties with the objective of taking these technologies to the underserved patients in the developing regions.
This could include the state sector, NGOs, or even commercial organizations. Affordability of the technology or device is another key factor that needs to be considered. This needs to be considered together with a scale of deployment. And I believe that healthcare is a fundamental requirement of all people and telehealth is the key contributor to making healthcare accessible for all. Healthcare systems must be reoriented to address NCDs. Today’s universal health coverage offers a global vision for healthcare systems. Achieving universal global coverage primarily depends on people-centered primary healthcare. All the more important, in the context of rising rates of NCDs affecting high income and low and middle income countries alike. In other words, to be effective, health systems must be rooted in the communities they serve and be able to not just prevent and treat NCDs, but also improve wellbeing and quality of life.
Maria Palombini
I think that’s a very important point that you’ve shared with our audience, and I hope that they embrace it when they’re developing their technologies or trying to deploy a device in those regions. Pramuka, a special thank you for joining me today.
Pramuka Sooriyapatbandige
Thank you very much. It was a wonderful opportunity for me as well, joining this session.
Maria Palombini
For all of you out there. As I mentioned, Pramuka is an undergraduate student in Sri Lanka. If you would like to see his actual pitch video from the IEEE SA Competition or any of the other winners and finalists, you can visit ieeesa.io/telehealthcomp. You’ll see highlights from the competition and everything about that.
Many of the concepts that Pramuka brought up today, we address in various ways throughout the IEEE SA Healthcare and Life Science practice. The mission of the practice is engaging multidisciplinary stakeholders and having them openly collaborate, build consensus, and develop solutions in an open standardized means to support innovation that will enable privacy, security and equitable, sustainable access to quality care for all.
Some of these activities that we have such as incubator programs for WAMIII, Wearables in Medical IOT, Interoperability, Intelligence, and Transforming the Telehealth Paradigm are addressing the many things that we discussed today from accessibility to security, to integration, to interoperability, to scalability, to extensibility.
And these groups are volunteers from all over the world, trying to build frameworks for potential global standards to address these issues. If you would like to learn more about these projects and many of the other practice activities you can visit our website at ieeesa.io/hls.
If you enjoy this podcast, we ask you to share it with your peers, colleagues on your networks. This is the only way we can get these important discussions out into the domain is by you helping us to get the word out. When you are using the podcast and sharing it with your colleagues, please reference #IEEEHLS or tag us on Twitter @IEEESA or on LinkedIn @IEEE Standards Association when sharing this podcast information.
I wanna thank you, the audience, for listening in today. I wish you all to continue to stay safe and well until next time.
Episode 4
Health Has No Borders with Telehealth – A Doctor’s Perspective
The need to extend telehealth services to marginalized and indigenous populations with a focus on accessibility and feasibility is urgent. As a primary care doctor converted into a healthtech advocate, Dr. Keith Thompson, shares that the work of equally reaching all populations for quality access to care will take more than setting up and/or relying on physical location.
Speaker
Keith Thompson
Chief Medical Officer, Nuralogix
Dr. Thompson is a London, Ontario-based family physician, graduate of the Schulich School of Medicine and Dentistry at Western University and awarded Fellowship Canadian College Family Practice in 2005. He is a Board-Certified Medical Affairs specialist.
He is an Adjunct Faculty Professor with the Western University Department of Family Medicine. At Western, he serves as Co-investigator on 2 virtual care studies and is a Medical Mentor for the Medical Innovation Fellowship program at WORLDiscoveries.
Dr. Thompson was one of the initial Canadian Physicians hired to consult with the Teladoc/BestDoctors Canada start-up team in February of 2018 and worked as CMO for iTelemed, a telemedicine startup in Ontario, prior to his recent appointment with Nuralogix.
He is a current member of the IEEE SA Telehealth Industry Connections Program, IEEE New Jersey Coast SIGHT (Special Interest Group for Humanitarian Technology), World Congress of Family Doctors (WONCA) eHealth Working Group, Association for Corporate Growth Toronto Chapter, Digital Health Canada, C.D. Howe Institute, and Co-Founding Member of Health Technologies Without Borders.

Full Transcript
Maria Palombini
Welcome to the IEEE SA Re-Think Health Podcast Series. I’m your host, Maria Palombini. I am Director Healthcare and Life Sciences Global Practice here at the IEEE Standards Association. This podcast takes industry stakeholders, technologists, researchers, clinicians, regulators, and more from around the globe to task.
How can we rethink the approach to healthcare with the responsible use of new technologies and applications that can afford more security, protection, and sustainable, equitable access to quality care for all individuals. You can check out our previous seasons on ieeesa.io/healthpodcast.
So as a result of the recent pandemic, the term telehealth has become a frequently used one and it does not appear to be going away. The reality is the way we see telehealth today will look very different. Telehealth is manifesting in many different forms. It’s more than what we commonly see as the doctor patient exchange on an audio/video platform.
It is so much more than that and continues to evolve with innovations in RPM, remote patient monitoring. The telehealth experience has changed the patient’s expectations on healthcare services. They’re relating to it more of a concierge level of online retail experience: convenient, appropriate, and personalized.
And then there’s this growing RPM space. There’s so many different forecasts when it comes to RPM, anywhere from 150 billion U.S. Dollars by 2028 to estimates of 40% of patients using one or two more of these devices at one time. But one thing is for certain, regardless if we are talking telehealth, mobilized health or RPMs, the future of delivering healthcare is not confined to a facility.
It will need to be patient-centered. Season four of this podcast series, Telehealth’s Quantum Leap into Patient-centered Care, talks to the innovators, the winners of the IEEE SA Telehealth Virtual Pitch Competition, the industry leaders, the clinicians, and other researchers who are at the forefront of driving innovation with solutions on accessibility, human factor design, flexibility, security, inclusivity, and all the other necessary ingredients to migrate healthcare to a patient-centered care system.
So just a short disclaimer before we begin, IEEE does not endorse or financially support any of the products or services mentioned by or affiliated with our guest experts in this series. It is my great pleasure to welcome Dr. Keith Thompson, Chief Medical Officer of NuraLogix Corp to our conversation.
NuraLogix was one of the nine finalists to make it to the pitch round of the IEEE SA Re-think the RPM Machine Virtual Pitch Competition. NuraLogix is an AI-powered solution for instant health and wellness data from your smartphone. I love this line on their website, so I’d like to share it with you all. It says: take a selfie to know you’re healthy.
And obviously Keith will share with us what that means. But in the meantime, one of the reasons why I really enjoy having Keith on this podcast is that he is co-leading a Pre-standard Work Stream, entitled Virtual Care Lexicon in the IEEE SA Transforming the Telehealth Paradigm Industry Connections Program.
So Keith, welcome to our podcast!
Keith Thompson
Thank you. Great to be here today. Really appreciate this opportunity.
Maria Palombini
Keith, you have a very well-established career in primary care as a family physician. You are an advocate for utilizing virtual care and telehealth to reach patients. You have demonstrated passion in helping patients in everything from WONCA, the World Organization of Family Doctors, but really what inspires you about the opportunities of virtual care? Most doctors are slower to technology adoption and you seem to embrace it so well. How did you get involved?
Keith Thompson
Thanks, Maria. I’ll be honest. I was really a late bloomer to technology and I jokingly say at this stage of my career I haven’t a lot of time left, so I have to make the best of it, but just seeing the advancement of technology and where workflows were going and how we were embedding this into our day to day encounter just really fascinated me. And obviously you start to see ways of doing things better.
Maria Palombini
Like they say, better late than never. So I’m so glad you migrated to it.
Keith Thompson
Yeah, absolutely.
Maria Palombini
So can you just briefly share with our audience the goal of the work that you had started with the virtual care lexicon work stream? Are you looking to standardize and how will it positively impact the future of telehealth and virtual care?
Keith Thompson
I came to IEEE as a clinician. So just to clarify, I’m not an engineer by any means, but love what it has done just hanging out with this group. It’s an interesting combination of the humanistic and sort of the artisan form of interacting with patients, but that zero room for error and an effort to try and make things perfect. The lexicon that was started really under the IEEE Telehealth Industry Connections that I came to, not really knowing what I was getting into, initially, it has become what started as an attempt to define telemedicine, both technically and use cases and specifically terminology.
And I see where we’ve moved more recently is into that realm of culture and linguistic appropriate services. How do we make this encounter better for the people that we’re trying to engage? And so how we can use that ICT, you hear that term Information Communication Technology, using it in healthcare, but an effort to connect both the materials for health and device literacy, the other area we’re getting into. It’s connecting those educational materials on a system like GUDID, the Global Unique Device Identifier Database, and there’s really a disconnect there. So we realized the first step within the lexicon, we hope to eventually get to a PAR in this class or culture linguistic appropriate services and, or the health and device literacy. Both of those are getting traction.
We’ve begun to explore some collaboration here in Canada, actually with indigenous communities. There’s some interest in the language resurrections and the standards that might result in making that telemedicine encounter culturally safe for first nations. And this is a huge part of what’s going on here in Canada, as we’re in the midst of reconciliation within our indigenous community.
So a project like this within our lexicon really might not only provide an output for standards around connectivity and databases. And what would this look like? So we can share that information with others, attempting to do this, but here in Canada, be incredibly healing, part of a supportive measure just to make telemedicine or virtual care culturally appropriate specifically for indigenous communities.
Maria Palombini
I think that’s a fascinating project and it can transcend many different ways across geographic and other aspects as well.
You went from doctor to Chief Medical Officer of a cutting edge technology company. So NuraLogix uses AI and machine learning, and it offers patients this ability to take a selfie and determine their level of wellness. Just for our audience, what exactly is it monitoring? What area of the population pool does it really serve and what makes this platform so unique?
Keith Thompson
I’ve recently come to NuraLogix and my background was within telemedicine. I’m a primary care doc first and foremost. So my day job is seeing patients. So my side gig was boring and trying to get some telemedicine endeavors off the ground.
We had a working relationship with NuraLogix and I was immediately fascinated. I was like, wow, this takes telemedicine to the next level. Being able to grab patient parameters and some biometric measures within that encounter. So the technology is a novel form of RPPG called Transdermal Optical Imaging and TOI is our trademark terminology. So by capturing blood flow, using that principle of reflected light, we’re not just measuring one region with TOI. We’re actually measuring 21 regions in the face and each region of the face acts differently. Your cheeks behave differently than your nose and your forehead.
So we’re able to capture that pulse wave form and then do feature analysis using machine learning models that are trained on 40,000 patients. And we can capture those patterns in the data sets that allow us readings on over 40 to 30 or more parameters for patients being scanned. So we’re able to capture vital signs, metabolic biomarker risk, cardiovascular risk, mental health stress related to HRV variability, and metabolic risk for diabetes of lipids. So our blood pressure is really our crown jewel. We are engaged with the FDA in a pre-submission. So our claims on this measurement still have to be validated as we get into that territory of class two medical devices. So you’ll see a disclaimer everywhere for investigational purposes only.
That’s really why we’re about to start clinical trials. We’re pretty confident with the technology. We’ve published data verifying that we can meet the ISO 81060 standards. And so can claim accuracy on that. And we have also published some data on our biomarkers of mental stress. The population that we’re serving really the intended use is to screen for risk factors and chronic disease states, under the care of a physician.
We’re not trying to replace the lab or replace the doctor encounter, but just build that awareness. So our solution can really identify if you’re at risk for cardiovascular, hypertension, diabetes, mental stress, heart rate variability and so many metabolic risks as well that we capture.
We’re soon going to launch hemoglobin A1C, an elevated morning fasting blood sugar. So it’ll be a classifier model. Yes, no. Are you above or below a certain level? And if you look at the World Health Organization, it really identifies hypertension type two diabetes and mental stress. Those leading causes of morbidity mortality.
You can see that we’re focused with our solution on those major epidemiological indicators for NCDs, you’ll hear this term Noncommunicable Diseases, and that’s really the big push. So we want our platform hopefully to be available to as many people as possible so they can understand and just be aware of their own health risk.
And we hope to identify those populations at risk before disease develops or its related complications. So the first step in health literacy really is awareness and that’s where we intend our tool to be used.
Maria Palombini
I think that’s really important. And I think you already touched on a misconception that we often hear, oh, I’m using these wearables and it’s monitoring me. So maybe I don’t need to see the doctor as often. And it’s like, no, this is supposed to be in support of.
Keith Thompson
Yeah, yeah.
Maria Palombini
So yeah, important. And it comes right from the doctor’s mouth. We hear a lot about patient centered care and patient centered this in the healthcare system. So when you think of remote patient monitoring devices, systems transforming, or trying to get to this patient-centered care system, where do you think there’s more attention needed or innovation needed to really transition RPM into a true patient centered care model?
Keith Thompson
Honestly, so many things come to mind. I think for me, and really I have to give IEEE and some of the mentors I’ve been working with credit for this, but the first thing that comes to me is equitable access. So what we’ve seen such a digital divide in society is we become more technology based. Yet those social determinants of health in which you hear about have really also become digital determinants of health.
They’re one in the same. The UN declared internet access as a basic human right, almost 10 years ago and we’ve made great strides in improving connectivity in internet access, but there’s still significant disparity, especially within those low middle income regions and marginalized populations where it’s either complex care needs, high urban density or folks with disabilities.
So the application of monitoring systems to the patient point of care, I think will move care closer to the patient in terms of capturing data. But then what sort of ecosystem and workflow are we creating in conjunction with the physicians embedded into that remote patient monitoring workflow and will we see the need for physicians in that workflow at all?
Will patients still want some sort of humanistic attachment and I’ve been diving into a thought leader here; she’s since passed away Ursula Franklin. She was an archeologist by trade, but released a whole thought process around technology. And she talked about technology being either prescriptive, right?
There are rules that you must follow or humanistic or holistic. And really medicine, when you think of it, certainly primary care, is holistic. So how do we combine those two things? And how much can we transfer over to the technology side and at what cost are we losing the holistic aspect? Also, just to comment that healthcare access really is only 25% of those health outcomes. In other words, getting access to healthcare doesn’t solve those issues around social determinants of health, which play a far bigger role in health outcomes. So improving those social determinants is needed, providing the technology or access to care just with technology may not achieve that end result or outcome that we’d expect.
So I think remote patient monitoring also points us to an era of high volume and low physician touch, which I say physician specifically, because there’s another technology thought leader here, Marshall McLuhan kind of another philosopher. He said that the age of technology will be the age of do it yourself.
That’s so true and we see as the knowledge in technical skills are now prescribed or advanced to systems. It could be a Google search to determine my symptoms or at some point AI or machine learning control of robotic surgery or diagnostic systems we’re already seeing. I think there’s a lot of unanswered questions as things go forward, but equity of access for sure is a key ingredient we have to maintain.
And I think that’s what IEEE and SIGHT and HAC have really been focused on and really passionate about. And it’s been great working with this group.
Maria Palombini
Absolutely. It’s really interesting though, you mentioned the social determinants of health. In season three, AI for Good Medicine, I actually interviewed the CTO of Closed Loop AI and one of their core projects on COVID 19, like the effective risk and outcomes was using data of social determinants.
The idea was to really look at the social determinants rather than just therapeutic risk based factors that really improve the outcomes.
So we prefaced this a little bit, but there’s a lot of misconceptions around, you know, remote patient monitoring devices. You know, patients are not going to adhere, the data can’t be validated, this thing is only gonna do so much. When you think about it, what do you see or what do you think is one of the biggest misconceptions when it comes to the concept of telehealth, whether it’s from a patient perspective, a physician perspective, the payers, or any other stakeholder in the process?
Keith Thompson
I think I may be biased from where I am as a physician, but for me, the biggest misconception might center around workflow. For telemedicine to be truly sustainable for physicians and payers, for that matter, it needs to be efficient and optimized in terms of workflow. So this means it supports both patients and providers so that they’re both literate and trained in the pre-visit, during the visit, and post-visit follow-up. What does that workflow look like? How much can we do digitally? Via surveys, questionnaires is a translator needed, is connectivity appropriate? What digital modality is best video or telephone, and does a patient have access to that modality?
I feel there’s some misconceptions maybe from payers, just how much time is involved in a good telemedicine encounter. So even without telemedicine, EMRs (Electronic Medical Records) have significantly increased physician admin burdens, right? The time we spend, we see so much greater integration of technologies to improve the depth of that encounter and using virtual care tools, but we increase the clicks, the log ons several minutes added to that encounter. So how do we cover that added admin time with limited healthcare budgets? So we’re expanding the non-clinical part of that encounter. There’s a disconnect really between the system designers and payers and patients’ and providers’, real world experience.
So payers, providers and patients that digital journey that everyone goes through to access and provide care experience firsthand, go through it. Co-design is so important. Right? So what’s the actual experience for all these actors coming into the system?
Maria Palombini
Absolutely. And I think these are all relevant points, because we all think, oh, we have a new technology tool. It’s gonna make everything go faster. But the transformation is not just the technology, the digital side of it. It’s the whole process that has to be aligned with it. Otherwise maybe we’re just making more work for all of us in the process.
So I often say, I write about this, I talk about it that the future of telehealth will look very different than we see it today.
As a physician, I think for you, why is it important to envision a potential future of mobilized care? We hear about the tele ICU in the future, the mobile urgent care units, but this idea of bringing healthcare to the home, how do we really see it improving patient outcomes?
Keith Thompson
It’s an interesting question, Maria, and I think the question really challenges us to look more closely at telemedicine virtual care and its applications under the same lens that we would use for other interventions, i.e. Pharmacoeconomics right. We talk about human economic outcome or health economic outcome research and cost benefits, cost effectiveness, cost utilization cost minimization.
So cost minimization, assuming that the outcomes are equal, but we can deliver care cheaper or maybe there’s benefits in terms of lower hospitalization. So you can see moving patients into home. Absolutely, one or two days saved from a hospital admission saves thousands of dollars or reduced ER visits. Cost effectiveness is more in actual natural units. So would an intervention, lower blood pressure, and there’s studies on this, right? By partnering with patients digitally, you can prompt them to take their blood pressure meds, to exercise, behavioral change, and we can see effective gains. Lastly, cost utilization, that’s quality adjusted life years, and that’s harder to put a dollar value on, right.
Is that ease of, of access, not having to travel to the doctor and, and all that. That’s convenient. So I think we have to be careful that not all care transitions to virtual in a cost effective manner, we might, for example, see physicians order more needless tests to compensate for that insecurity, a lack of an exam.
And some studies have hinted at this. On this angle, patients might feel that seeing more than one physician just due to ease of access. And I had that counter, you know, with a patient coming to see me and saying the video assessment wasn’t really an exam doc. I needed somebody to listen to my lungs. Right. So we had two visits that could have been done in one. I think we’ll need to apply a little tougher if you look at the economic lens and it makes everybody cringe because we know the convenience. We know the patient’s love of, of ease of access and lower costs for physician encounters. For sure. But in the global economy, what does it look like?
Yeah, we may have to be careful.
Maria Palombini
Yeah, absolutely. We kind of just touched on this before, but we hear of oh, we’re bringing healthcare into the home. Right? Do we really still need doctor’s offices and hospitals and you sort of just led into that. But the real question is, how is that dynamic changing in this area of healthcare? Right? Like thinking of the hospital as the place to go for care.
Keith Thompson
There’s so many forces at play here. And certainly there is in the medical system and physicians, especially in primary care, we want continuity and longitudinal relationships. The patients want convenience of access in some ways opposing forces. Right? So I, I believe the hospital’s always gonna be the go-to for surgical treatments, radiotherapy, for example. But days in the hospital will no doubt be shorter. And I think the post-operative timelines move into the home with less inpatient time. So the question, or perhaps the danger is, is going more into remote patient monitoring and home based care. How far is a physician interaction with its patients removed from that digital ecosystem?
You saw one of my recent posts on LinkedIn, right? With an RPM system that got hacked. You could do a whole thing on security. I’m sure. All the actors weren’t notified, but the poor docs and nurses involved for that remote, fetal heart monitoring, the system was down.
Nobody knew. Patient didn’t know, physicians weren’t notified, and there’s gonna be a really messy lawsuit as a result. The other part to this, how much of that face to face is therapeutic, and really can’t be replaced by a digital workflow. And I’m not sure we know the answer to that yet, but there’s one person that can tell us and that’s the patient. Just, as I mentioned before, about Ursula Franklin, you know, that prescriptive force of telemedicine and remote patient monitoring becomes so strong that this becomes now the only way of doing things. And so i.e. that digitally and remote patient monitoring fewer face-to-face visits, but how holistic and compassionate is that healthcare system, will it be at that point?
We can, yes, have ISO 9000 perfection and supersede that need for human touch and interaction with patients, you know, how far do we go and who knows, certainly this is where we need to dig down. I think a bit more and perhaps further research on patient reported outcomes and satisfaction and not just healthcare dollar saved.
Maria Palombini
Absolutely. And I think it’s an important point that we always talk about stakeholder trust and everybody thinks well, will the patients trust the process and the device, but we also need the doctors and the clinical workers to trust it as well. And so if workflows are not designed to best mitigate risk for all the parties involved, then we’re gonna continue to have this question of trust.
Keith Thompson
I wish honestly, every one of my colleagues could at least do a couple of stents in some of our meetings to learn about that issue. I trust that my device is measuring properly. I have no idea the standards and the protocol for that trust. And I can think differently about calibration now and how I approach, you know, just simple measurements.
Maria Palombini
So we’re kind of leaning into this question here and I think you mentioned it as well earlier on, this question of health equity, right. We know there’s marginalized populations without access to healthcare, or very limited access to healthcare or understanding of the healthcare process. So telehealth technically right should reach those who are the hardest to reach.
Keith Thompson
Yeah.
Maria Palombini
So Keith, in your view, how can telehealth equitably reach the patients who are currently not included in the healthcare system. What do you see as some of the challenges that need to be addressed? Obviously you mentioned the language was one, but that telehealth could be a viable platform to try to close this healthcare gap.
Keith Thompson
As I mentioned earlier, those social determinants become digital determinants. They become one in the same in my opinion, but apply that technological access to a marginalized population doesn’t unto itself, improve an outcome. Certainly, access I think is the cornerstone. We’ve gotta have a secure line into those communities and it should be a basic human right just as clean water and food security. And beyond this, I think then we look to focusing or leveraging community health workers within those communities. You know, we’ve had some presentations here with IEEE Public Health Foundation of India and Dr. Aaron Jose and their telemedicine program.
Look it up, doing some great work, partnered telemedicine with community workers, right. To be that line in. We partnered at NuraLogix with LaFiya to put telemedicine kiosks into remote regions of Nigeria. What’s interesting about that platform is the solar panel that they put in that community is being used as a resource to provide some micro economies that might be the alternative business model, because really the issues move away from solving the connectivity to solving those social innovations and business models to support those regions. So there’s no longer value in the model of just selling devices and multiple units to providers or consumers rather, how do we fund a single device and platform and scale to regions needing support for tens of thousands of patients without access to primary care. The technology’s great, but we really have to keep our eyes on the ball I think on the sustainability and business model, because it’s certainly talking about compassion and humanitarian reach. I think you’re sort of assuming that it’s for free and it’s, you know, NGO and it’s a philanthropic offering, but there’s ways to do it right. That we can support communities with technology and help them sustain themselves.
Maria Palombini
Absolutely. Very, very good. All right. So Keith, you’ve given so many insights. I think your perspective as a physician working in a really technical environment is really, really refreshing. Any final thoughts you would like to share with our audience? It could be technologists who are embarking in virtual care technologies or already there and looking at this context of patient set and care, it could be a call to action, a call for attention and innovation.
Keith Thompson
Yeah. You know, really honestly, just to say thank you to you and IEEE, right? That industry connections and SIGHT, this organization has been an incredible mentor and inspiration for me.
I’ve said that combining engineering design with zero error and medical humanitarian applications, right? Compassionate care here has been an incredible journey. So call to action. Get involved in this organization, if you can, you’re gonna grow personally and professionally. And I guarantee, you know, become a better person just by helping address those needs of humanity using technology and last thanks to NuraLogix for supporting me in this right.
They’ve encouraged me, no questions asked. I love it. So great. I really appreciate Maria. Thank you.
Maria Palombini
Thank you, Keith, you always got so many great insights, your passions, and, you know, for humanitarian causes and just overall, just your empathy for patients. It’s just very refreshing.
So thank you for taking the time and being part of this podcast today.
For all of you out there, if you wanna learn more about NuraLogix, you can visit nuralogix.ai. If you would like to get involved in the work stream, Keith mentioned virtual care lexicon, or other aspects of the IEEE SA Transforming the Telehealth Paradigm Incubator Program, visit ieeesa.io/telehealthic.
Many of the concepts we talked about today with Keith are addressing so many different activities here at the IEEE SA Healthcare Life Science Practice. You know, the mission of the practice is engaging multidisciplinary stakeholders, such as Keith and they openly collaborate. They build consensus and develop solutions in an open standardized means to support innovation that will ultimately help us achieve the goal of privacy, security and equitable, sustainable access to quality care for all.
Activities such as the Transforming the Telehealth Paradigm, the WAMIII, Wearables and Medical IOT, Interoperability Intelligence are just naming a few of the different activities here. And if you wanna learn more, how you can get involved, there’s no cost to join these activities, you can visit ieeesa.io/hls.
If you enjoyed this podcast, we ask you to share it with your peers, your colleagues on your networks. This is the only way we can get these important discussions out into the domain is by you helping us get the word out so you can use the #IEEEHLS or tag us on Twitter @ieeesa, or you can tag us on LinkedIn @IEEE Standards Association when sharing this podcast.
So a special thank you to you, the audience, for listening in today and continuing to stay safe and well until next time.
Episode 5
Securing the Telehealth Experience is Critical for Patient-Centered Care
Security and protection of personal data are core tenants in driving trust in the use of remote devices and technologies for monitoring or delivering virtual care. As healthcare intersects more with consumer wellness trends, the vulnerabilities and threats to security and privacy are even more amplified.
Nakia Grayson and Ronald Pulivarti from the National Cybersecurity Center of Excellence (NCCoE) at NIST, share the latest trends and efforts on how the industry is educating and offering practical guides to safeguarding the telehealth experience.
Speakers
Nakia Grayson
IT Security Specialist, NIST/NCCoE
Nakia Grayson is an IT Security Specialist who leads Supply Chain Assurance & Autonomous Vehicle project efforts at the National Cybersecurity Center of Excellence (NCCoE), which is part of the National Institute of Standards and Technology (NIST). She is also a part of the Privacy Engineering Program at NIST, where she supports the development of privacy risk management best practices, guidance, and communications efforts. Nakia serves as the Contracting Officer Representative for several NIST cybersecurity contracts. She holds a bachelor’s in criminal justice from University of Maryland-Eastern Shore and a master’s in information technology, information assurance and business administration from the University of Maryland University College.

Ronald Pulivarti
Healthcare Program Manager, NIST/NCCoE
Ronald Pulivarti is the Healthcare Program Manager who leads the Healthcare team at the National Cybersecurity Center of Excellence (NCCoE), which is part of the National Institute of Standards and Technology (NIST). He and his team promote the acceleration of businesses’ adoption of standards-based, advanced cybersecurity technologies for the healthcare sector. Mr. Pulivarti has a strong technical background and cybersecurity experience in multiple high-value asset applications. Prior to NIST, he worked within the Department of Health and Human Services and has served in many IT leadership roles for over 20 years.

Full Transcript
Maria Palombini
Welcome everyone. This is the IEEE SA Re-think Health Podcast Series. I’m your host, Maria Palombini, Director of Healthcare and Life Sciences Global Practice here at the IEEE SA. This podcast takes industry stakeholders, the technologists, researchers, clinicians, regulators, and more from around the globe to task.
How can we rethink the approach to healthcare with the responsible use of new technology and applications that can afford more security protection and sustainable equitable access to quality care for all individuals? You can check out our previous seasons of the podcast series at ieeesa.io/healthpodcast.
So as a result of the recent pandemic, the term telehealth has become a frequently used one and it does not appear to be going away soon. The reality is, the way we see telehealth today will look very different tomorrow. It’s manifesting in many different forms. It’s more than what we commonly see as the doctor/patient exchange on an audio/video platform. It can be so much more involved with innovations in RPM (Remote Patient Monitoring), mobile health, hospital at home, and many different areas. The telehealth experience has changed the patient’s expectations on healthcare services. They’re relating it more to a concierge level, online retail experience: convenient, appropriate, and personalized.
And there’s the growing RPM space. So many different forecasts when it comes to RPM, anywhere from U.S. 150 billion by 2028 to estimates of 40% of patients utilizing one or two of these devices at one time. But one thing is for certain, regardless if we’re talking telehealth, mobilized health, RPMs, the future of delivering healthcare is not confined to a facility and will need to be patient-centered.
Season four of this podcast series, “Telehealth’s Quantum Leap Into Patient-Centered Care,” talks to the innovators, winners of our IEEE SA Telehealth Virtual Pitch Competition, the industry leaders, clinicians, and other researchers who are at the forefront of driving innovation with solutions on accessibility, human factor design, interoperability, security, inclusivity, and the other necessary ingredients to migrate healthcare to a patient-centered care system.
So just a short disclaimer, before we begin, IEEE does not endorse, advocate, or financially support any programs, services, technologies mentioned, or affiliated with any of the experts who have appeared in this series. And with that out of the way, it is my pleasure to welcome Ronald Pulivarti, NCCoE (for those out there, National Cybersecurity Center of Excellence), Healthcare Program Manager and Nakia Grayson, NCCoE IT Security Specialist. The NCCoE is part of the National Institute of Standards and Technology, NIST. Welcome, Ron and Nakia!
Nakia Grayson
Thank you to IEEE for inviting us to do the podcast interview. And thank you, Maria, for hosting the interview. We are so excited to be here today!
Ronald Pulivarti
I’ll echo that. Thanks a lot for having us and to the IEEE community. We appreciate the opportunity to do this podcast with you, and hopefully we’ll be able to engage deeper and we can get some great learning from our conversation.
Maria Palombini
Absolutely. I think for our global audience out there, this is gonna be a great experience. Before we get to the core, the technology, what’s going on. I like to humanize the experience for our listeners, right. We’re all in a virtual world. So Nakia, you started out in a different role while at NIST and then transitioned to an IT Security Manager.
What inspired that change? What do you love about the work you are doing now?
Nakia Grayson
Before we begin, Ronald, I would like to just say that opinions we are going to share in this podcast are our own and not the opinions or positions of NCCOE and/or NIST. So to answer your question, yes, that’s correct. I started off in a different role at NIST and actually in an administrative role and later transitioned into IT Cyber Security role in 2018.
For my undergraduate studies in college, I majored in criminal justice. When I graduated, I really wanted to bridge my education and knowledge of the legal system with a career in technology, policy, and privacy, because since I’ve, you know, found all of those areas, I was already fond of those as a teenager. While working in a lead administrator role at NIST, I went to graduate school for Information Technology and while in school I became really interested in data protection and cyber security risk management and how both of these play a very important role in protecting and safeguarding the nature of critical infrastructure and privacy and sensitive data.
I really love working on this. NIST gives me the opportunity to work alongside world class talent and industry experts to tackle and solve the most complex problems in cybersecurity and privacy.
Maria Palombini
Excellent. Well, Nakia. We have a lot in common because I also did my undergraduate in criminal justice, but again, I didn’t go that path either. But an unbelievable opportunity to be working at the forefront on cybersecurity issues.
So, Ron, how about you? I understand that you’ve had an exciting professional background working in organizations, such as Health and Human Services ,the HHS. What have been some of the most exciting areas of your work? What would you say are some of the major compliments you have seen during your tenure?
Ronald Pulivarti
It’s quite interesting. I’m a technology nut, so one of the things that I’ve always actually noticed when I started at HHS is I was the guy picking up the support phone. So from understanding the nuts and bolts to actually managing these ecosystems has been such a great opportunity. I’ve been able to launch myself throughout different agencies within the HHS space. I was able to contribute and strengthen the technology foundation so that we could grow. And one of the big things that I felt like I was able to provide in this space was my technology experience. I see something and I think five years to 10 years ahead on where we should actually be. And I think one of the things or opportunities that I enjoy doing was taking a look at the current snapshot on where things are, and actually contributing and making a significant impact within the government space so that we can advance and we can grow and strengthen the government technology, workspace, and ecosystem.
And I enjoy it each and every day.
Maria Palombini
That’s awesome. We all know that we have to love what we do otherwise it really will feel like a job. And then that is not the point.
All right guys. For our audience, you got a little insight to our background and to the things that really motivate our guests today.
So let’s get to the core. Nakia, we hear about all kinds of risk in the remote patient monitoring ecosystem. What are some of the major risks you are seeing that can no longer go unaddressed? In simple terms, what exactly are we up against?
Nakia Grayson
Some of the major risks that we’re seeing in the RPM ecosystem, speaking from an organizational standpoint that can no longer go unaddressed, is when HDOs deploy RPM solutions.
These solutions are architecture that includes several components across the HDO, the telehealth platform providers, and the patient’s home. So each of these environments is managed by different groups of people and often with different sets of resources and technical capabilities.
So risk can cut across the architecture and the different methods by which one may mitigate those risks. And it can vary based on the complexity of these. So while HDOs do not have the ability to manage and deploy privacy and cyber security controls, they do oftentimes retain the responsibility to ensure that the appropriate controls and risk mitigation are applied.
So in simple terms, a lot of data is being transmitted back and forth across various platforms which can lead to access points to cyber criminals . So we need to ensure that we have the appropriate controls in place. The safeguard systems look deeper in the current infrastructure as technology advances, ensuring that we also have education training for our patients.
Maria Palombini
Yes. I think that’s a very important point, Nakia, because we all think that it can just be a simple apply, a patch and let’s move on. We really need to talk about the whole scope of what it takes in security. And that includes educating patients, because a lot of them might be completely oblivious to what’s going on.
So Ron, we’re seeing growing trends of non-clinical, let’s call ’em consumer-issued health IOT devices, being utilized by patients. They share with their health providers. With this new integration, what kind of security and privacy risks are to be considered?
What are some possible solutions? Do we rely on the healthcare delivery organization, the device maker? Who needs to step up and start creating some solutions here for all this data in these devices.
Ronald Pulivarti
Very good question, Maria. One of the things that we all need to really consider and think about is that as these devices are evolving, they’re constantly listening to us, right?
So understanding exactly the use of it and what we’re using it for and applying that privacy and security standard on how you wanna communicate outward. So understanding your surroundings is a critical aspect of that. And all of the groups need to be involved from the technology provider, from the HDO, even from the consumer.
Understanding the layout as we do every day rely on our technology IOT devices to turn on lights, we rely on it to turn on and adjust the thermostat. These are constantly pinging in our whole household. One of the most important pieces for our project, our remote patient monitoring project in our appendix E in our practice guide, we actually talk about the benefits of these IOT devices.
We provide the device capability mapping, the device capabilities that support these functional evaluations. But one of the big things that we really need to factor in is what means of communication are we using this device for and what safeguards can we put in our own house with communicating, whether it’s medical information, personal information, when you’re talking to your bank. You have to utilize that space to ensure that if these devices are constantly listening to you, where is the safest part in your house, that safe house? And you could actually have these communications without exploiting any information that you have.
As Nakia pointed out, there are bad actors every day. We’re constantly fighting them. So using those steps, I think in place to understand that there’s a constant chatter that’s happening in the background. Where is that safe place in your environment where you could actually utilize these devices to ensure that you’re safe and you’re properly communicating things without necessarily having someone intercept something in some form or fashion?
Maria Palombini
And that’s absolutely a great point because I think in this world of everything “smart:” smart thermometer, smart this, we talk about ease and convenience and all these great things, but patient beware, right? You have to understand that all this “smartness” also comes with a lot of insecurity.
And so the same way you won’t leave your front door open, we really shouldn’t leave these kinds of things so open and vulnerable as well.
So Nakia, Ron, sort of, he did mention the guide. So I know that you all released this Securing the Telehealth Remote Patient Monitoring Ecosystem Practice Guide. Our team, the IEEE SA Transforming the Telehealth Paradigm Group, read it once it was released. We saw it was a bunch of great diverse companies involved in helping you guys create this project.
So can you share with us the supporting laboratory project around it? What was the idea? Was it tested in the lab environment to actually get to the final guide? Share with our audience the making of this guide.
Nakia Grayson
We get so pumped up when we have the opportunity to share our work. It’s great to hear that IEEE has found our work very useful. So the use of healthcare delivery organizations, HDOs, rely heavily on telehealth and remote patient monitoring (RPM) capabilities to treat patients at home. That has increased.
And some of the reasons why, is because RPM telehealth service is convenient and cost effective for all parties. And that’s the HDO, the telehealth provider, and patient. And one thing that we always want to share is that there are many actors in the RPM environment and that’s the HDO, the telehealth provider, and the patient.
So in our practice guide, we assume that the HDO’s engaged with a telehealth platform provider that is a separate entity from the HDO and patient. The telehealth platform provider managed distinct infrastructure applications instead of services. The telehealth platform provider, they will coordinate with the HDO to provision, configure, and deploy the RPM components to the patient home. Also assure secure communication between the patient.
We analyze the RPM ecosystem risk factors by applying methods to describe and our NIST risk management framework. We leverage the NIST cybersecurity framework and our NIST privacy framework, and other relative standards to identify measures to safeguard the ecosystem. In collaboration with healthcare technology and telehealth partners.
We built out a RPM ecosystem and a laboratory environment to explore methods to improve the cyber security of a RPM. So we brought in different technology from vendors to build out this lab. In our practice guide, we make a note that the application of people, process, and technology is very important in having that risk mitigation strategy.
So in our practice guide, the benefits that we stress is that we want to help an organization ensure the confidentiality, integrity, and availability of a RPM solution and enhance patient’s privacy and limit HDO risk when they are implementing a RPM solution.
Maria Palombini
I know that the telehealth guide was really thinking about the RPM in this environment. And this is where we are right now, but we know the trend. We hear it coming about bringing hospitals to the home and everybody’s thinking, this is the future. But how can the work of this practice guide be either applied in some form to address what we think is going to be a huge appealing, uh, cybersecurity appetite for the hospital at home concept?
Ronald Pulivarti
We’re a non-regulatory agency, right? So our practice guides are free for using it as a guidance for especially our targeted audience of these small and large scaled organizations. The way our practice guides are carved for folks to use, we have three different volumes in our practice guide.
We have our Volume A, it really talks about our executive summary of our remote patient monitoring. Then our Volume B is pretty much good for the actual overall architecture. It provides our approach, the architecture, the security characteristics. And then Volume C is really our how-to guide. We provide detailed instructions, how to implement our solution.
One of the things you touched on that’s very important is what was it back then to where we’re going to now. Telehealth is gonna be a very near to never going to go away type of technology. We’re gonna be utilizing this forever until something else new pops up. But I would highly encourage the folks to visit our website.
Our website is nccoe.nist.gov. So it’s nccoe.nist.gov. We have our practice guides that are listed for folks to take a look at and our remote patient monitoring practice guide is there. And Nakia has touched on it, it has valuable bits and pieces of information on the types of work that we’ve actually done specifically for this project.
Maria Palombini
Absolutely. Actually this podcast series, season two was all about cybersecurity and connected health. And all of my guests from around the world really never said it outright, but every time I asked them the question, it seemed like more, they were addressing the issue in the form of mitigation of risk in the connected health system.
So when we talk about cybersecurity talking more security or the mitigation of risk? The idea of a solution that someone’s going to develop someday can never be breached. Is that too much pie in the sky idea?
Nakia Grayson
I really like this question. As we sometimes look at these things as being different, we believe that we’re talking about the same thing. They work in conjunction. So privacy and security work hand in hand. Cyber security is more focused on the physical devices and privacy is focused more on the data.
But I think we’re talking about the same thing. You just really want to get to what is the best thing that we’re trying to provide? What are the solutions that we’re trying to assure that HDOs and small companies can do? And one thing that we mentioned is our practice guide is a great tool to be used to improve cyber security and posture and potential data risk when it comes to the telehealth ecosystem.
Maria Palombini
Absolutely. We didn’t go too much into privacy in this conversation, but they do go hand in hand for sure. Ron, what do you envision as the next best steps in attempting to better secure and protect this RPM ecosystem? We’re seeing more devices enter the healthcare sector with all these cool, smart features such as AI at the edge, that are not only gonna do monitoring, but at some point they’re going to make autonomous decisions without a human intermediary. So I imagine the risk level just goes up a little more in those kinds of scenarios.
Ronald Pulivarti
That is absolutely correct. One of the big and most important pieces here with the project and as we’re entering into new devices in our own home or different environments is understanding those risks with that architecture. We provide our privacy framework, cyber security framework, our risk management framework.
There are so many opportunities for learning to understand that level of risk. And one of the other pieces here is ensuring that your HDO as you partner with the right telehealth platform provider to extend that privacy and cybersecurity control deployment management and efficacy. One of the things that are out there is we’re constantly evolving in technology.
So you need to consider future technologies that can augment data communication safeguards. Also Maria, I will end off on this last note, which is important. Our website, we are actually pushing more and you touched on the word AI. We’re exploring so many different capabilities that are out there within the national cybersecurity center of excellence that consumes not just our remote patient monitoring piece, but we have different areas within our center. We have 20 active projects, for example, over at our center that we’re constantly looking for collaborators in. So one of the things that when, and if folks get the opportunity is again, check our website and look underneath the security guidance tab. And you have different areas by different sectors that we are looking for collaborators in.
We publish information out. We look for feedback as your comments are very valuable for us to constantly improve our information as we’re rolling it out for consumption. So take a look at that underneath again, the security guidance tab, we have different sectors that are available and as we’re evolving in different types of technologies and those areas of interest, we have our practical, usable, repeatable guides that are there and also we love feedback. So there’s a community of interest distribution list under each of these sectors. Do register. Be part of our experience to help improve our current infrastructures that exist today.
Maria Palombini
Absolutely. Last season was AI for Good Medicine. We had so many great different use cases and ideas there. We’ll make sure our guests and our audience are aware of these other opportunities at the NCCoE.
You guys have shared so many great insights with us already. You know, the guide I think is awesome.
I’m gonna pose this question to both of you and I’ll ask Nakia to go first. Any final thoughts you would like to share with our audience as it comes to developing remote care technologies under the context of patient-centered care? Any interesting upcoming projects, plans of action? Things just to think about in general? What is your parting final thought Nakia ?
Nakia Grayson
So I would say that if you haven’t already checked out a RPM Practice Guide 1800-30, we definitely would encourage everyone to read it, check it out. And if you have any project ideas to contact our team. We would like to mention that when we published our RPM practice guide, we also published two tip sheets focused on telehealth. One is for the patient and one is for the provider. Each tip sheet includes a couple of strategies on what each can do. As far as the patient, the provider, to mitigate cyber security and privacy risk or other telehealth services.
And I’ll turn it over to Ron to share about upcoming projects.
Ronald Pulivarti
Thanks, Nakia. Yeah, Maria, we’ve actually had two great virtual workshops. We had one just recently was the virtual workshop on our smart home integration project. The turnout was phenomenal. We had a lot of speakers. We had technology providers, health delivery organizations there to contribute, and we had an open panel discussion. That was wonderful.
Aside from that, we also had our exploring solutions for cybersecurity of genomic data. That was a two day workshop we had. We provide a lot of information for individuals that are registered in our community of interest for each of our different sectors, register! As we have more and more virtual webinars, and hopefully sooner than later physical workshops together. We send out communications and we post it on our website. So register for a community of interest so you’d be notified whenever we have our webinars or workshops. You will also get the opportunity to be part of our draft guidance for the public to consume and provide feedback. You’ll be notified whenever we need comments. So please do so. A lot of these projects that we do here, we try to make it very informative for people out there that actually need to have some type of guidance or some type of framework.
And because we’re such an organization where we rely on collaboration, it’s very important to get people to get involved with us. So once we’re in our labs, once we’re together, we can really do a deep dive and really figure out where these problems reside in which we can actually provide some type of output for a solution that folks outside of our lab can actually, um, use.
Maria Palombini
Absolutely. I mean, I subscribe when I get those updates as well. The IEEE SA volunteers and various projects have responded to NIST calls for feedback and that kind of thing. So for our audience, whether you’re with us or you’re on your own, definitely we are in many ways involved in trying to help the overall global community address these big challenges that we’re facing.
Ron and Nakia, thank you so much for joining me today. It’s been an absolute pleasure.
For all of you out there. If you wanna learn more about all the work going on at the NCCoE at NIST I say, all roads lead to the website, nccoe.nist.gov. All the information, as Ron and Nakia mentioned, is free for you guys to consume. I think it’s a great resource if you’re in this space, whether you’re technical, you’re innovation, you’re a clinician. I think it’s valuable for anybody to read it.
A lot of the concepts we talked about today are addressed in various activities throughout the IEEE SA’s Healthcare Life Science Practice.
Our practice is really engaging multidisciplinary stakeholders from around the globe who openly collaborate. They build consensus and develop solutions in the form of open standardized means to support innovation that will address these issues of privacy, security, and equitable, sustainable access to quality care for all.
Some of our programs: Transforming the Telehealth Paradigm Industry Connections Program and WAMIII, which is where both Medical IOT Interoperability Intelligence cuts to the core of a lot of the discussions we were having today. If you’re interested in learning about these projects and all the other areas we’re involved in, you can visit ieeesa.io/hls.
So if you enjoy this podcast, we ask you to share it with your peers, your colleagues, through your network. This is the way we can get these important discussions and ideas out into the domain, is by helping us get the word out. Be sure to use the #IEEEHLS or tag us on Twitter @IEEE SA.
Special thank you to our audience for listening in, continue to stay safe and well until next time.
Episode 6
Reimagined Healthcare: A Personalized Concierge Virtual Care Experience
Telehealth is disrupting the traditional healthcare experience of hospital fee-structured models to help better address health inequity. As one of the leading telehealth platform providers, Teladoc’s Medical Officer, Dr. Shayan Vyas, shares how achieving a deep understanding of patients’ behaviors and needs cannot be fully addressed in the traditional healthcare setting.
Learn how the customized patient experience that can be enabled through telehealth technologies is feeding the future of “the hospital at home” and healthcare consumerism.
Speaker
Dr. Shayan Vyas
Medical Officer, Hospital and Health Systems, Teladoc
Dr. Shayan Vyas is a critical care physician as well as an experienced physician executive with a successful track record in healthcare innovation particularly digital and virtual medicine. Dr. Vyas is Sr. Vice President at Teladoc Health, where he serves as the chief medical office for Teladoc’s hospital and health systems. Teladoc supports over 600 health systems globally for their virtual care with Teladoc’s software, hardware, and services. During his tenure at Teladoc, he has overseen physician management, physician relations programs, as well as product development and clinical quality. From medical care to creating innovative IT design, and SaaS sales, he is skilled in physician workforce management, leadership, and healthcare. He has proven success in building and maintaining relationships with physicians and other healthcare stakeholders that increase revenue streams. Dr. Vyas is also an active board member, advisor and mentor to several healthcare software & hardware companies. Prior to joining Teladoc, he was the Executive Director of Telehealth at a very large multi-state multihospital health system. He also is faculty at the University of Central Florida College of Medicine. Dr. Vyas He received his medical degree from Medical University of the Americas and his master’s in business administration from Auburn University (Harbert College of Business).

Full Transcript
Maria Palombini
Hello everyone and welcome to the IEEE SA Re-think Health Podcast Series. I’m your host, Maria Palombini, Director of the Healthcare and Life Sciences Global Practice here at the IEEE Standards Association. This podcast series takes industry stakeholders, the technologists, the researchers, clinicians, regulators, and more from around the globe to task, we ask them how can we rethink the approach to healthcare with responsible use of new technologies and applications that can afford more security, protection, and sustainable, equitable access to quality care for all individuals?
We are currently in season four, but you can check out our previous seasons on ieeesa.io/healthpodcast. So we all know as a result of the recent pandemic, the term “telehealth” is frequently used and it does not appear to be going away soon. The reality is that the way we see telehealth today will look very different tomorrow.
And it’s manifesting in many different forms. It’s more than what we commonly see or think as the doctor/patient exchange on some sort of audio or video platform. We look at innovations in RPM, remote patient monitoring. We look at how telehealth experience has changed even the patient’s expectation on healthcare services relating more to a concierge level, online retail experience, convenient, appropriate, and personalized.
And with this growing RPM space, there’s so many different forecasts when it comes to it anywhere from U.S. 150 billion by 2028 to an estimate of 40% of patients may be utilizing one or two of these devices at one time. But one thing is for certain, regardless if we are talking telehealth, mobilized health, or RPMs, the future of delivering healthcare is not confined to a facility. It will need to be patient-centered.
So season four of this podcast series, Telehealth’s Quantum Leap into Patient-centered Care, talks to the innovators, which are the winners of the IEEE SA Telehealth Virtual Pitch Competition, the industry leaders, the clinicians, and other researchers who are at the forefront of driving innovation with solutions on accessibility, human factor design, flexibility, security, inclusivity, and any other necessary ingredients to migrate telehealth care to a patient-centered care system.
A short disclaimer before we begin, IEEE does not endorse for financial support any of the products or services mentioned by or affiliated with our guest experts in this series. And now, it’s my pleasure to welcome Dr. Shayan Vayas, Senior Vice President and Medical Director of Clinical Operations at Teladoc Health.
Shayan was also a judge and advisor on the IEEE SA Rethink the Machine: Transforming RPM into a Patient-centered Care System Virtual Pitch Competition. And he’s also a participant in our Transforming the Telehealth Paradigm Industry Connections Program. Welcome Shayan.
Shayan Vyas
Thank you very much, Maria. It’s a pleasure to be here with you and IEEE listeners.
Maria Palombini
Before we get started to the core of the awesome work that’s going on at Teladoc, Shayan, you started with a successful career as a physician and you transitioned to virtual care and IT design. What was the catalyst for this change?
Shayan Vyas
Being a critical care physician, I’m at the frontline with the team, treating the sickest patients in the hospital. It’s the most vulnerable time for patients and families. This experience taught me a lot about obviously medicine and really the patient experience, but also mortality. As we think about how technology transsects patients, physicians, and clinicians, it significantly helps them, but it also can overburden them.
Furthermore, clinical care or even just bedside medicine is a model of one to one. I deliver care, clinician or nurse delivers care one to one and that’s not scalable. Even during my early training, when I was doing missionary trips as a young clinician, I wasn’t well experienced and I was still learning the art of medicine.
I wasn’t typically seeing bread and butter illnesses. And at this time, I really started to begin valuing and using technology. Phones started having the capabilities of doing video visits pretty easily and it’s become part of our everyday life.
That moment when I used the device to be able to call my mentors and my coaches back home during these trips, I realized this could be a catalyst. This could be a transition of how one to one can be one to many; how others can be impacted if I’m in another world, another country delivering care, and I’m able to connect to specialists and mentors back home, how can this affect the patient?
Technology can redefine the world we live in. We’ve seen that with innovators like Steve Jobs, Bezos, think about that with healthcare. There’s gotta be a way where we can take IT design and virtual care and just redesign the world that we live in, in healthcare.
Maria Palombini
Absolutely. I remember we were having a meeting one day in our telehealth group, and you just said something in passing, but it caught my attention. And I remember you vividly saying that tides have turned. No longer is the patient’s health experience like beholden to the times when you go to a doctor’s office and you have to sit there for hours, waiting for them to let you in. Like a patient’s demands are changing. And they want that concierge level experience as they get with retail. So how do you see telehealth overall, trying to meet that changing need?
Shayan Vyas
Patients are patients, but in this context, let’s say the word consumers, right?
So patients/consumers, they’re bringing their everyday expectations from other industries into healthcare. They’re intersecting their experience when they shop online or they stream a movie or even buy an airline ticket into healthcare and other industries. That experience that they enjoy and have the flexibility of doing in entertainment or shopping or whatnot, they’re starting to expect that in everything that they do. When’s the last time the listener actually went to the airport to buy a ticket? When’s the last time the listeners actually went to a store and rented a movie? That haul has changed. Even more, if you’re outside of a very large city, like New York, I’m in now, when’s the last time you actually flagged down a cab or you drove to a restaurant to carry out? Those things, they’ve revolutionized the world we live in. They can be done on an app or a browser. And that same consumer experience is what folks are craving when it comes to healthcare.
Consumers/patients, they don’t wanna wait in waiting rooms anymore. They don’t wanna wait six weeks for their PCP to send them to a specialist. Telehealth is just the beginning of this transformation. It allows that one to many that I described earlier, but more importantly, it’s starting to meet the bend of what consumers are demanding. I think this transformation of healthcare is just getting started. The in person aspects of medical care or going to the doctor will be held for the very few life threatening procedural needs.
I really believe that the tide has changed in that healthcare historically was built around the doctor, my waiting room, my parking lot. You’re gonna go on my terms, it’s changed to the patients. Patients now can schedule visits, they can go and look up what medical school I went to and what my press community score is. They can now shop around and that power is obviously well deserved. Consumers should know where they’re walking into. They have the right to choose what movie they wanna see, they can see the reviews and what others have said about it. The same thing should be in healthcare.
The tides have changed.
Maria Palombini
Absolutely. I think we get caught up in everything and sometimes we don’t realize that because innovations are coming out so fast, we lose sight of some of these things.
So Teladoc is one of the top 10 telemedicine companies founded in 2002. There’s rankings all over on the internet, but it’s always in the top 10 and that’s 20 years ago. The world really wasn’t talking about telehealth, nowhere near at the level we do it today and it’s actually only the publicly listed telemedicine company. So obviously the pandemic catapulted, the use of telehealth out of necessity. However, Teladoc was already on its way.
Do you find that Teladoc’s success is founded on its principle, that it’s a patient-centered platform?
Shayan Vyas
Absolutely. 20 years ago when Teladoc started, our physicians were actually breaking the law. We were taken to court and we ended up counter suing my home state, the board of medicine there.
And we changed the way society and law looked at a physician and a patient relationship. We did that because it was all about the patient-center. We wanted patients to have access to healthcare 24/7 without having to leave their home. In my mind, that ruling and the fundamentals of our company changed the balance of the physician “owning” the individual patient.
And it allowed now the patient to really understand and own their journey when it comes to healthcare, their choices, their flexibility. This is a transformation in not only just the law, but medical economics, and the fundamentals for consumers, obviously that propelled us to be the first publicly traded company and really the largest virtual company in the world.
It’s all about the patient. We have to deliver high level quality care. That’s an expectation that is a basic need in healthcare. Patients deserve to get the highest quality of care, but changing the principle around and delivering a platform that the patient can control was fundamental.
Maria Palombini
I think often we see innovations coming out and it’s all about, oh, the next best shiny thing. And it can do this and that, but we lose sight that we’re still serving the critical need of the patient. And I think this is really interesting. So for all you out there, Telehealth Doc, this was just released publicly. They signed a partnership with Northwell Health. And for those of you outside the New York Metro area, Northwell Health represents, one of, I think, New York’s largest healthcare provider. And the goal is to better provide access to virtual care across its enterprise. So we definitely focused on the patient, but one of the things, when we think of telehealth services, we think it’s easy, right. You just plug into a platform, turn on the mobile device and let’s connect and, obviously have the doctor/patient experience.
What are the considerations for the workflow from a physician’s perspective that must be changed to accommodate this transition to virtual care?
Shayan Vyas
A comment on Northwell, they have one of the greatest CEOs in the healthcare world ever. Very great organization. Over 18,000 physicians. They’ve been practicing telehealth for a long time.
When it comes to accommodations to transition to virtual care, there are multiple consumers that are using the platform. There’s the health system. So the administrators from the health system need to have data. There are physicians and now nurses and all kinds of clinicians are working. So we’ll use the term clinicians and then there’s the patient. There’s the IT team.
And so all of these consumers need to be thought of. So when we first started out, as mentioned previously, we built a platform really around the patient, but now there’s multiple end users that need to be thought of. You gotta think about those that we just mentioned. And in terms of thinking about how to transition everything to virtual care, the bar to virtual video visits is very low.
There are many ways to do a virtual visit now. You can do it essentially for free now with any app, to connect with grandmother or to connect with colleagues around the world. That bar is now very low. Everyone has a video platform. The bar to scalability is very hard. The bar to interoperability within multiple EMRs.
I think Northwell has 22 hospitals, 830 facilities, the integration in and out of the firewalls and in all the data systems that they’re using, that’s the hard part. And then when you multiply it, we have over 600 health systems around the world that we work with.
That is really hard in terms of just the individual physician’s perspective to replicate the in person experience or has to make it much easier.
Physicians are wasting a lot of time today with stuff that is not really adding value to the patient, the care they’re delivering, or even the ROI that the health system is investing in. And so when we think about adding video conferencing, it’s not just that. You have got to amplify the ability for folks to be able to practice at the highest level of their license.
Maria Palombini
It’s very interesting that you mentioned that because I was talking with Dr. Keith Thompson, who’s also part of the Telehealth Program and he said almost the exact same thing from a clinician perspective. As doctors we’re getting in all this administrative action outside of actual care action, helping the patient because of all these changes in workflows. And he was saying that this is where it’s really important to understand what the doctor needs to focus on and what the patient needs to focus on. And then let the experts handle all that other stuff.
Shayan Vyas
Here’s the reality, right? As an intensivist, I have a different perspective than an ambulatory physician, but even as an intensivist, I spend maybe 10% of my time at the bedside. The other 90% is I’m a data clerk. I’m entering data into an accounting ledger. It’s not making patient care easier. It’s not making the care safer.
It’s really a billing machine. And when you talk to my ambulatory colleagues, they’re doing the same thing, right? They’re spending minutes. I think that the average family practice doctor spends eight minutes with a patient. And they spend 30 minutes just charting and documenting and clicking here and there. As a consumer, I would rather a clinician spend 30 minutes with me and then the eight minutes doing the charting that adds no value to the system, but is where all the money and the transaction occurs.
Maria Palombini
I’m sure patients would agree with you 100% on that point.
So as we move towards greater adoption or use of virtual care, more acceptance, how do hospitals best negotiate the balance of patients expectations for home care versus hospital facility care? They are significantly different, but we still have patients’ expectations when they’re not doing well. So how does that balance work out?
Shayan Vyas
Maria, this is a great question. So let’s take a step back. The origin of modern day telehealth started really with employers and health insurances. They wanted to figure out a financial way to lower the delivery of care. The emergency room versus a telehealth visit is significantly cheaper for everybody. Significantly easier if you can get your symptoms and your illness resolved that way. That’s really where it started. It was really around the payers. Regarding hospitals, they get paid for beds and heads. It’s a very common term. We’re in a fee for service world. And the best way to get paid is when you have a head inside a bed.
When you look at health systems like Northwell Health, Kaiser Permanente, Intermountain, they have moved out of this fee for service world where they no longer are getting paid based on every procedure they do. The fee for service industry itself has plagued healthcare. You go to a surgeon, they’re gonna operate on you because they get paid that way.
That’s the way the model was. There was no value incentive for a surgeon not to operate on you. And so as we move from this fee for service world and to this value based world, that’s where we start to move the needle. The financial incentives now to actually do what’s in the patient’s best interest, try to deliver on this expectation that consumers or patients have in home care versus hospital care.
That’s where we start to see the needle move as more and more health systems start to develop MA plans and they start to take financial risk. They’re starting to think about how they can move away from bricks and mortar care to virtual care. That’s easier for everybody, it’s cheaper for everybody. And that’s how it’s gonna happen.
I think health systems are gonna have a hard time to be honest, trying to deliver full based virtual care when they’re fee for service. It’s not the same. It’s dollars to pennies when you meet in person versus you see me in virtual, in that fee for service world, but in that value based world, as long as I deliver the care, no matter if it’d be virtual or in person, delivering that care is what it’s at.
Patients are expecting that virtual visit when they go to the doctor or they have a surgery and they wanna do that visit. It’s a standard that a patient expects. But again, there’s a balance of getting paid and when health systems and physicians are getting paid more in person than virtual visits, then that’s a challenge.
It’s hard to move the financial needle that way. But as health systems and CMS are starting to push really for this value based care will really exponentially propel telehealth and virtual care.
Maria Palombini
I think that’s a really important transition that I think the whole industry needs to better evaluate and keep an eye on. I often say, and I talk about this with many different volunteers here at IEEE SA about the future of telehealth looking very different than it does today. And as a physician, why is it important to embrace the migration towards virtual care? The idea of bringing healthcare outside of the facility to the home and can it really improve patient outcomes? Can it actually better serve patients across the board?
Shayan Vyas
Before virtual care or even telehealth or remote patient monitoring, the standard for any of us was to go into the doctor, the bricks and mortar doctor. What did we learn from that? We learned that those that had access got better care. The proof is here. Everyone knows about DNA and genetics and hereditary diseases. Today 60% of health outcomes are determined solely by one thing. Do you know what that one thing is? Zip code.
Maria Palombini
Interesting.
Shayan Vyas
Not your DNA, not how long your parents lived, not the cancers that are in your family, but zip code is the primary determiner of your health outcome.
That’s fundamentally flawed. For those that live in a poor area, rural area, those determinants, what we call social determinants of health, access to fresh groceries, clean food, all of those things, high education, good paying jobs. Those are all social determinants of health, but when it comes down to access and one’s health, it was zip code.
And so as we think about this migration of virtual care, no matter where you live in this country, no matter where you live in this world, you can get access to Mayo Clinic. You can get access to. Kaiser to Northwell to all of these health systems. And that’s changed the game when it comes to access.
As we think about this embrace migration towards virtual care, I think that patients are gonna get better outcomes. That’s just the start of it. So there’s factors out there like the digital divide, not every American has access to high broadband, but those are being addressed. When we think about 60% of one’s health is determined by just your zip code.
We can change all that with virtual care.
Maria Palombini
Wow. Just the zip code. It’s so astonishing to think about. And I think this leads to my next question on health equity. Especially as there are marginalized populations without access to healthcare for a whole myriad set of reasons, but telehealth technically should reach those who are the hardest to reach. So in your view, how can telehealth equitably reach the patients who are currently not included in the healthcare system? What do you see as some of the challenges that need to be addressed so that telehealth could be a viable platform to close this healthcare gap?
Shayan Vyas
I think this is the golden question that a lot of CEOs, health systems, and those in the ecosystem are trying to address. We mentioned one of those barriers is zip code, but also the digital divide. Almost two out of 10 Americans don’t have access to broadband. Telehealth equity needs to address that.
It’s one of the main reasons that we merged with Livongo almost two years ago. Livongo was the first publicly traded chronic disease management company. What made them very successful and continues to help us grow is that all of the devices within that are sent to the patient doesn’t matter if they have access to broadband or not.
Why? Because they’re cellularly enabled. There’s cellular chips in the device, right? So glucose is checked for diabetics. The glucometer is the device that actually checks the glucose. Those devices have cellular chips in them. So we are automatically connecting these patients no matter where they are cellularly.
As we think about those that don’t have access. You gotta design it. We’re talking to the future entrepreneurs, engineers of the world. You have got to think of the basic connecting blocks when it comes to patient care. And so that was an MVP. Livongo started to make sure that the devices were all suddenly connected.
When you think about the scale of what we do at Livongo, we are now able to predict what folks’ glucoses will be, or predict mental illness for patients. And so, that’s the full spectrum that needs to really be addressed when you think about a viable platform that can help close the healthcare gaps.
Maria Palombini
I think that’s really interesting and I think you started the segue to my final question. You’ve given us so many great insights and talking to you is always an educational experience.
Any final thoughts, Shayan, about what you would like to share with our audience as it comes to really developing virtual care technologies under this context of patient-centered care; maybe it’s a call to action or a call to think about innovation in a different way.
Shayan Vyas
First off, Maria, thank you. I appreciate the invitation. I hope so far that it’s been insightful for your listeners.
Here’s my call to action or innovation: spending in the United States’s Healthcare System doubles every 13 years. The healthcare industry today is over 3 trillion (U.S.) dollars. If we continue, we’re gonna destroy the economy. There will be no social security, no retirement, the investments that we’re trying to make in our infrastructure, in our children’s lives, that will all be robbed to pay for healthcare. And so we have got to jump on this. I’ve never been more excited about healthcare and innovation. I’m excited. I believe in Moore’s Law, that technology dramatically increases in power and decreases in cost and that’s what gives me hope.
As you and I continue to age and when we get sick one day, we would love that technology to be “Uber” easy, right? Travis Kalanick with Uber, Elon Musk, Jeff Bezos, and Steve jobs- they were able to transform the world we live in into just a new experience that 10 years ago, we wouldn’t have even experienced.
I remember my mom would tell me, don’t get into somebody’s house that you don’t know. We do that with Airbnb. My mom also told us not to get into a stranger’s car. Now we’re calling strangers to pick us up. And so if you think about how those transformative leaders really recreated the world we live in, I’d love for your listeners to stay curious.
Think about equity when it comes to all people and don’t accept the status quo. The way we do something today is not okay. Think about how you can transform the world. If you stay curious and you have that open mindset that you want to help everybody, not just the financially well off, and you really challenge what we do, why we do this today, don’t accept those things.
So I hope that’s motivation and I’m looking forward to watching IEEE help a lot of startups and entrepreneurs. And I appreciate the opportunity. Thank you, Maria.
Maria Palombini
Thanks, Shayan, this has been really great. It’s really interesting you mentioned aging. We just started an activity for telehealth around robotics to support the aging, healthy, and assisted living for the exact same reason. I think we are expecting our aging population to outpace our younger generations, for sure.
Again, special thanks to you, Shayan, for joining me today, it’s been an absolute insightful experience.
Shayan Vyas
Appreciate it. Thank you.
Maria Palombini
And for all of you out there, if you wanna learn more about Teladoc Health, you can visit teladoc.com
Many of the conversation concepts we had here today with Shayan are addressed in various activities throughout the Healthcare Life Science Practice. The mission of the practice is engaging multidisciplinary stakeholders and have them openly collaborate, build consensus, and develop solutions in an open standardized means to support these goals around innovation that will enable privacy, security, and equitable, sustainable access to quality care for all.
Programs such as Transforming the Telehealth Paradigm, WAMIII, which is Wearables and Medical IOT, Interoperability, and Intelligence, and a whole host of other things on Decentralized Clinical Trials and Digital Therapeutics for Mental Healthcare.
If you wanna learn more about these projects and all these different activities, you can visit our practice website at ieeesa.io/hls. If you enjoy this podcast, we ask you to share it with your peers, colleagues in your networks. This is really the way we get these important discussions out into the domain is by you helping us to get the word out. You can use #IEEEH LS or tag us on Twitter @IEEESA or on LinkedIn @IEEE Standards Association when sharing this podcast.
I wanna do a special thanks to you, the audience, for listening and continue to stay safe and well until next time.
Episode 7
More than Skin Deep: Remote Probing to Detect Cues Before they Surface
Skin health, wound care and management are critical concerns for caregivers, long-term facility staff, and patients. Most often, damage to skin has not been detected until issues have already progressed.
Dr. Sanna Gaspard, CEO and Founder of Rubitection, shares how the latest in RPM innovations offers a non-invasive, on-demand monitoring capability to improve patient outcomes with treatment, care, and prevention.
Speaker
Sanna Gaspard
CEO & Founder, Rubitection
Dr. Sanna Gaspard is the CEO and Founder of Rubitection, a health tech startup whose assessment and care management platform support for chronic wounds and dermatological conditions can help improve patient outcomes and reduce costs. As CEO she oversees business strategy, partnership development, fundraising, product development, and marketing. Her vision is to make Rubitection’s solution globally available to empower anyone to assess and manage chronic skin conditions to personalize care. Her accolades include the 2022 Richard King Mellon Foundations Social Impact Award, 2021 Culture Shift Labs Innovation Competition, and ’19 AnitaB PitcHer winner, and ’19 Vinetta Project winner. She has a PhD in Biomedical Engineering with a Specialization in Medical Device Development from Carnegie Mellon University.
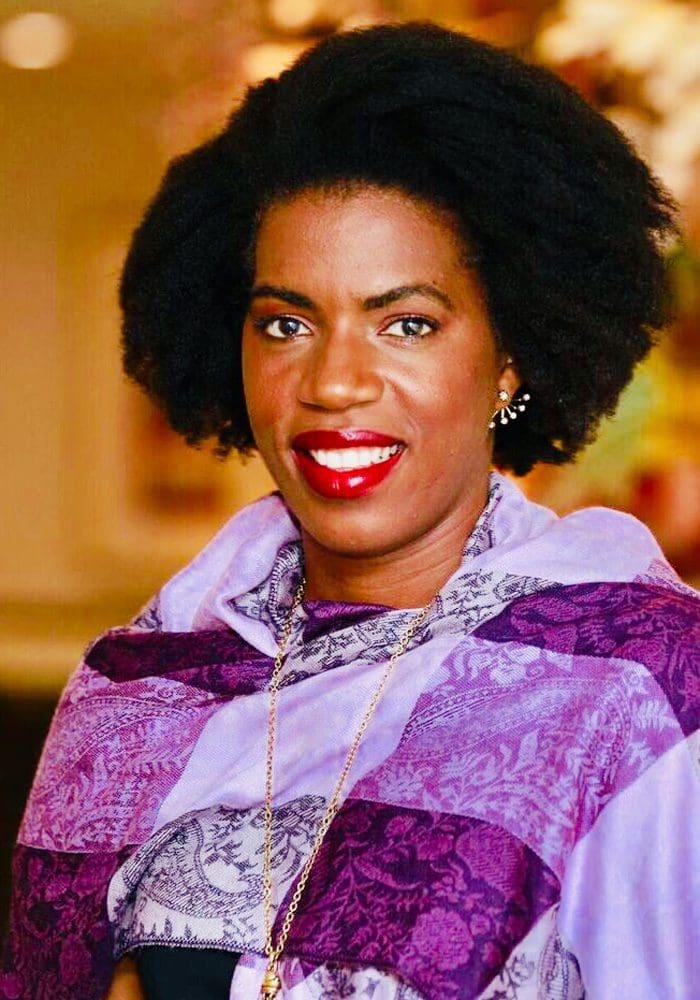
Full Transcript
Maria Palombini
Hello everyone and welcome to the IEEE SA Rethink Health Podcast Series. I’m your host, Maria Palombini, Director of the IEEE SA Healthcare and Life Sciences Global Practice. This podcast takes industry stakeholders, technologists, researchers, clinicians, regulators, and more from around the globe to task. How can we rethink the approach to healthcare with the responsible use of new technologies and applications that can afford more security protection and sustainable equitable access to quality care for all individuals?
We are in season four of the podcast series. You can check out our previous seasons on ieeesa.io/healthpodcast.
As we all know the result of the recent pandemic, the term telehealth has become one of the most frequently used ones, and it does not appear to be going away soon. The reality is the way we see telehealth today will look very different tomorrow. It’s manifesting in many different forms. It’s more than what we commonly see as a doctor/patient exchange on an audio/video platform.
It continues to grow, especially with RPM devices, Remote Patient Monitoring devices. The telehealth experience has changed the patient’s expectations on healthcare services. They’re relating it more to a concierge level, online retail experience: convenient, appropriate, and personalized.
And then there’s this growing RPM space. There’s so many different forecasts when it comes to RPM. Anywhere from U.S. 150 billion dollars by 2028 to estimates that 40% of patients will utilize one or more of these types of devices at one given time. But here’s one thing for certain, regardless if we’re talking telehealth, mobilized health, RPMs, the future of delivering healthcare is not confined to a facility and it will need to be patient-centered.
So season four, of this podcast series, Telehealth’s Quantum Leap into Patient-centered Care, talks to the innovators. These are the winners of the IEEE SA Telehealth Virtual Pitch Competition, the industry leaders, clinicians, and other researchers who are at the forefront of driving innovations with solutions on accessibility, human factor design, flexibility, interoperability, security, inclusivity, and any other necessary ingredient to migrate telehealth care to a patient-centered care system.
So a short disclaimer before we begin, IEEE does not endorse or financially support any of the products or services discussed by our guests in this series.
It is my pleasure to welcome Sanna Gaspard, CEO of Rubitection, Inventor of the Rubitect Assessment System to our conversation.
Hi, Sanna, welcome to our podcast.
Sanna Gaspard
Thank you for the opportunity. Looking forward to talking to you today.
Maria Palombini
I’m excited to have Sanna here with us! Rubitection garnered the first place position in the entity category of the IEEE SA Rethink the RPM Machine Competition.
So Sanna, before we get to the core of your innovation, tell us a little bit about you. You’re CEO, you’re an inventor of this solution, what drives your passion in your work? How did you get here?
Sanna Gaspard
What really drives my passion in my work is being able to innovate to improve healthcare. I have a PhD in Biomedical Engineering with a specialization in Medical Device Development and Commercialization. I came to that after thinking about being a pre-med to become a doctor and realizing that wasn’t the best career for my personality and what I wanted to do. I decided I really wanted to still have an impact in healthcare, but maybe on developing the technology that doctors use. And so now I’m just passionate about getting the technology out there to help caregivers and patients.
Maria Palombini
I think it’s fascinating because I’ve interviewed physicians who are migrating over to IT and Technology Design because they felt like, well, this is really what I wanted to do.
So we often hear that starting a company in this space derives from some sort of personal experience. Somehow they may have been afflicted, a family member, or something they came across doing university research. Is there a personal story behind bringing this innovative RPM approach to wound care? What was the vision and impact you imagined that it could have for patients?
Sanna Gaspard
So the personal story was really driven more by my desire to want to improve healthcare as a career than personal experience with the condition. I came across a condition while I was in grad school. At the time I was looking for a project where I could develop technology to improve care, but I really wanted to focus on something that was a healthcare problem, that was very common, but being overlooked.
And so when I learned about bed sores and I went and researched it, I found that it was killing like 60,000 people every year, affecting 2 million people per year, but the assessment approach was really still something that was manual where technology could be used to improve that assessment to save lives.
And so that was really what drove me to do that, I wanted to make sure that I spent the time on my PhD doing something that I could translate out to improve care and really address a real healthcare problem.
Maria Palombini
Absolutely. So it’s interesting, we often hear you need thicker skin to survive in this world. And in this case, you just mentioned 60,000 people die from complications due to bedsores every year, people think, oh, it’s just a little condition, but it does take people’s lives. That’s one person every nine minutes, so it’s pretty significant and over 55% of nursing home residents die from bed sores within six weeks of onset of the wound.
We all may have elderly relatives living in nursing homes, this is something we all have to consider. So let’s get to the core of the interview of how this RPM innovation can start to really have an impact.
Can you share the types of research, maybe some modeling in the years that worked, that went into developing this product? What would you say in your research was the most interesting piece of information that came through in this R&D phase?
Sanna Gaspard
The most interesting piece of information I would say was twofold. One, how long the problem was outstanding. There’s comments back to Florence Nightingale and I think even possibly some references in Egyptian literature to these wounds and bed sores. But there was no real solution at the time. And that was partly being driven by legislation and policy partly because a lot of the costs for those wounds was being covered by the insurance companies and Medicare. But as they’re providing primary care and the patient develops a wound, they would still get additional payments for that care. So for me, that was a striking thing that was driving a lot of the lack of innovation in this space. There was a longstanding need.
The other thing that really caught my attention was the importance of correlating the technological platform to the clinical environment and how important that would be. So when I first learned about the issue, I went and researched all the different technical logical approaches you could use like ultrasound spectroscopy ,temperature and tried to match that against the user needs in that environment to see what would be the most appropriate. And I found that really was an interesting exercise in terms of like someone who’s interested in developing tech, you can’t just go and say, oh, I think this is a tech I want to use or the technological platform I want to use to solve this problem. You really have to cross check it around what the users need and how it would integrate into that environment around usability and ease of use. That was a lot of the early work I did that drove the direction of the technology in terms of development.
Maria Palombini
There are many different skin conditions from eczema to bed sores to wound care. How does the RAS system work to identify the abnormality? And at the same time, how can it indicate what exactly is the abnormality? Like it’s a diabetic ulcer, it’s a bed sore, it’s a wound, whatever it may be.
Sanna Gaspard
The Rubitect Assessment System, abbreviated RAS, is essentially a device that helps to assess the skin to identify chronic inflammation or conditions in a dermatology space or in the wound care and surgical space. So in a dermatology space, it could be used for things like rosacea, eczema, eventually, maybe things like skin cancer for early screening and in the wound care space, we’re looking at diabetic foot ulcers, pressure injuries and surgical wound monitoring.
It essentially includes a software system that you can monitor data on and a device that you place onto the skin to make measurements of the skin, to identify areas of inflammation. So you place a device on the skin. It makes a measurement predominantly using optics, and then you get an assessment following that measurement about low, medium, or high risk or gives you a diagnosis.
And you can then share with your primary care physician to get an updated care plan or to understand the next steps in the care plan. Our real goal with that system is to really support effective early assessment to prevent the progression of advanced wounds or to help patients in a dermatological space, either do early assessment to evaluate treatment effectiveness based on the prescriptive treatment that their doctors provided so that they can support care compliance and using the system, or get a new prescription if that product is not working. On the wound care side, it’s catching it early to prevent advanced wounds that can be deathly.
Maria Palombini
Very interesting. So we’re trying to get ahead of the game here.
Sanna Gaspard
We’re trying to get ahead of the game and empower people.
Maria Palombini
One of the key features that you presented in the competition is that the data collected is interoperable with medical health records, which for patients, that’s a great opportunity. How have you seen physicians and caregivers use the data collected about the patient to sort of alter their care, to make it better and how does the data collected actually integrate into their patient’s medical chart?
Sanna Gaspard
So right now, we’re still in R&D. So we haven’t fully launched the product, but when we launch it, we depend on having an EHR integration. From a remote patient care standpoint, the measurements they do at home to provide a risk assessment or to do care planning and management would be sent back to their primary care physician.
Where they would confirm the data, confirm the care plan, and then also be able to save that in the EHR. When using an acute care setting, it would just be an inherent part of the EHR as they’re using the system. The data’s then also stored in the EHR for later data analysis or reporting and documentation.
Maria Palombini
We mentioned nursing facilities and long assisted living facilities. So one of the population sets that this may benefit is naturally the aging population. However, when we think about the aging population, they’re not usually considered the most digital and or trusting of these types of technologies.
What has been your experience or in research, being able to reach this age demographic, to utilize the RAS system, to trust it, to want to use it? What are some of the lessons that you might have learned through this engagement?
Sanna Gaspard
I would say some of the lessons I’ve learned through this engagement oftentimes is that you have to go through a family member or you have to go through their adult child.
Oftentimes their adult child is the person providing care or the nurse is the person providing care. So the main part of targeting this population is going through their care provider or their primary care provider, or the person who’s managing that care. And then basically working with that person to either explain the importance of the problem or how the technology can really help support them in managing that care.
But oftentimes getting access directly to those potentially elderly patients can be difficult, because you really can’t necessarily go to them directly. You have to go find their care provider.
Maria Palombini
Trying to turn caregivers into advocates for the use of this technology in order to help this area of the population.
Sanna Gaspard
Yes, exactly. And finding those caregivers in either advocate groups or finding those consumer targets in a home setting can be difficult. You’d have to go through the primary physician or the primary care provider. Basically go that way.
Maria Palombini
When we think of the pool of patients, it’s more than just the aging, because we’re talking a wide swath of wound care issues, other issues, diabetics. How do you see your technology being patient-centered? And when we talk about patient-centered it could be a point of accessibility, inclusivity, feasibility, adaptability. Is there a population of patients that you can better serve with this technology that perhaps could not be reached or accessed or included before when it comes to RPM opportunities?
Sanna Gaspard
We’re working on a skin health assessment tool that has applications in dermatology, in wound care, and surgery. In all of those fields for patients who have chronic dermatological conditions like psoriasis or eczema and even skin cancer, oftentimes, they would have to come into the office to get an assessment, or they were sending pictures or using really crude technology to try to document their condition to eventually share that with the doctor when they went into the office. Also true for patients with wounds so that when the patient goes home, their family members and caregivers are told here’s the care plan to help prevent this person from getting a wound but then they only see the doctor once the wound develops. So that makes prevention and early detection really difficult.
So really in each of those market segments, we are providing an access to a level of care that wasn’t available before, unless you went into the doctor’s office. So now you can have in-home monitoring to monitor changes in the skin to catch things early, share that with your physician, get an updated care plan, then catch things at an earlier stage when they’re least costly and the easiest to treat.
Maria Palombini
That’s a fascinating point. Because as a caregiver, you call a doctor and how you articulate something is not going right in a medical way. So I think this is a fascinating area because that is one of the caregiver’s biggest concerns. Can I take care of this at home? Am I capable of doing this? How about if something goes wrong? You get all these questions, right?
Sanna Gaspard
Exactly. And then in talking to caregivers in the home setting, another thing that comes up is like, as you’re responsible for that care for your loved one, your parent, your grandmother, maybe even a disabled child or someone with a chronic health condition, you’re trying to do your best to manage the care and manage your life. And when they get something that’s preventable, like bed sore that can be really severe. There’s a lot of guilt and shame associated with that oftentimes because they feel responsible and we really want to just help empower caregivers to understand that without technology, it is really hard to do that early detection and then to empower them to feel like they have the tools to prevent some of the chronic complications of a bed sore so that they can feel confident in the care that they’re providing in managing that care.
Maria Palombini
Absolutely. That’s a great benefit for caregivers out there. For sure.
As a tech startup, would you think of any technical standards, policies, opportunities, or something in place that would’ve made the development of this product go faster, easier. And after going through this process, what areas have you identified would open the doors to innovation in the telehealth space? And in your opinion, what would be the best way to address it?
Sanna Gaspard
One is funding because you need funding to be able to develop the technology. And I think having technical organizations that can support technical founders in getting access to funding or providing funding as investors or grants would be already a great start.
And I think also from a medical standpoint, technical standards around EHR integration would also be really helpful in meeting that HIPAA requirement because there’s so many ways, it’s usually customizable to each person’s technology, but having really clear standards about how you have that healthcare integration with each EMR systems would go a long way. Because all of the EMRs are slightly different, how you communicate with them in their platforms. And so it makes tech development with EHR integration very cumbersome and expensive.
Maria Palombini
So it’s almost like a tech entrepreneur mentorship sort of way of helping tech engineers. One being able to understand how to source and get funding as needed as they’re developing the product. But also understanding what tech guidelines are out there that maybe no one knows about, because we tend to always uncover these things and even say, okay, they’re not existent, but maybe this is something else you can use.
So I agree. I think there could be some definite guidance from people in that role before, and probably can point you in a faster, easier way to get to the answers you’re looking for.
Sanna Gaspard
Yeah, I would agree with that.
Maria Palombini
You’ve given us some really interesting insights, especially when it comes to this whole area of therapeutic on the health side and the opportunity of supporting the caregiver for which we don’t see too often in a lot of RPM devices. What is something that you would like to share with our audience? It is a diverse group. We have technologists, we have people in the clinical field. We have researchers, regulators, policy people, whoever’s listening to this podcast. What would you like to share with them when it comes to really understanding developing technologies under the context of patient-centered care?
Sanna Gaspard
I think the most important thing is that it takes everybody. Technology can’t be created in a vacuum. As someone developing technology, I need access to healthcare providers. I need access to the caregivers and patients to understand what their needs are. In terms of the clinical providers, I need access to them to understand clinical integration and use cases and how to ensure that the device meets usability requirements and also clinical integration requirements. Policy makers usually end up driving things around pricing and large market drivers that affect adoption around reimbursement or medical policies for use or requirements for use in reporting that really end up driving clinical adoption. And also things around regulatory issues like the FDA. So it really takes everybody and there should be really more groups where that brings together a diverse group of stakeholders that technologists can access in one place. So like right now, if I wanna talk to a doctor, I have to go and find a doctor. Then I have to go and find the patient in a different location. And I have to go find the stakeholder from a policy standpoint in a different location. There’s not one place that you can go and get a holistic view of the problem to get the perspectives of each major stakeholder in one setting.
Maria Palombini
I can see that, but that’s also symptomatic unfortunately, of the healthcare system, right?
Sanna Gaspard
It doesn’t have to be fragmented. I mean, people have historical data of their images of their personal life and we can’t manage to get longitudinal data of our own health.
Maria Palombini
That’s a very good point. Sanna, thank you so much for joining me today and sharing all these exciting insights.
Sanna Gaspard
Thank you as well for the opportunity. I enjoyed talking to you, and if anybody wants to reach out, they can shout to me at [email protected].
Maria Palombini
Absolutely. If you guys wanna learn more about the Rubitection Assessment System and about Rubitection in general, you can visit rubitection.com. And you can learn all about Sanna as well and her advisory team and all the other information that’s on there.
Many of the concepts we talked about with Sanna today are addressed in various activities throughout the IEEE SA Healthcare & Life Science Practice. The mission of our practice is engaging multidisciplinary stakeholders and having them openly collaborate, build consensus, and develop solutions in an open, standardized means to support innovation that will enable privacy, security and equitable, sustainable access to quality care for all.
And these are activities such as WAMIII: Wearables and Medical IOT Interoperability Intelligence Incubator Program, and Transforming the Telehealth Paradigm Industry Connections Program. And there’s a whole host of others in Decentralized Clinical Trials, AI, Digital Therapeutics for Mental Healthcare. So if you’re interested in learning how you can get involved or think about instantiating an activity, you can visit our practice website at ieeesa.io/hls.
If you enjoyed this podcast, we ask you to share it with your peers, colleagues on your networks. This is the only way we can get these important discussions out into the domain is by helping us to get the word out. Be sure to use #IEEEHLS or tag us on Twitter @IEEESA or on LinkedIn, IEEE Standards Association.
I wanna do a special thank you to you, the audience for listening in. Continue to stay safe and well until next time.
Listen On The Go
About the Host

Maria Palombini
Director, IEEE SA Healthcare & Life Sciences
As the leader of IEEE SA Healthcare & Life Sciences, Maria works with a global community of multi-disciplinary stakeholder volunteers who are committed to establishing trust and validation in tools and technologies that will change the approach from supply-driven to patient-driven quality of care for all. Her work advocates for a patient-centered healthcare system focused on targeted research, accurate diagnosis, and efficacious delivery of care to realize the promise of precision medicine.
Get Involved
If you would like to participate as a guest, underwrite the series, or share topic ideas, please email Maria Palombini.
Receive Updates
Stay up-to-date on new releases and related activities by subscribing to IEEE SA Healthcare & Life Sciences.
IEEE does not endorse or financially support any of the products or services mentioned by or affiliated with our guest experts in this podcast.